Robotic-assisted McKeown esophagectomy
Clinical data
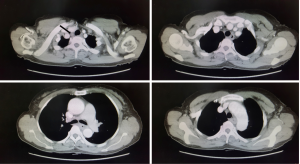
The patient was a 53-year-old woman with a history of dysphagia for 3 months without nausea, vomiting, hematemesis, or stomachache. A protruding mass was detected 25–30 cm from the incisors by gastroscopy. The pathological biopsy result was esophageal squamous cancer. The patient lost 5 kg without anorexia. A physical examination showed no positive sign, and results of preoperative biochemical tests were all normal. Enhanced computed tomography (CT) scan revealed a thickened upper esophagus wall and enlarged lymph node in the superior mediastinum (Figure 1). Informed consent for robotic-assisted thoracic lobectomy was obtained from patient before operation.
Operating steps
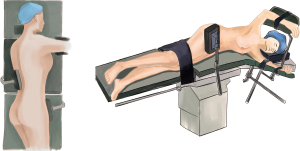
Anesthesia and position
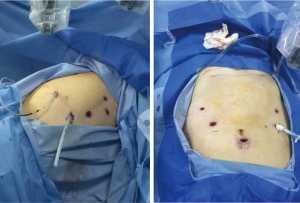
After general anesthesia, the patient was placed in a left lateral decubitus position with left one-lung ventilation in thoracic part (Figure 2). Supine position with two-lung ventilation in the abdominal part (Figure 3).
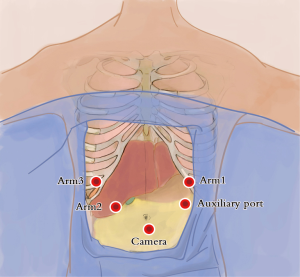
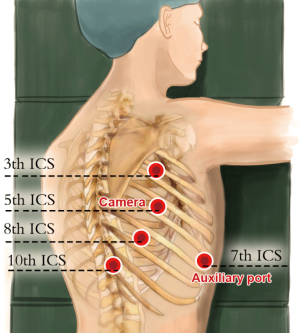
Ports
Abdominal ports (Figure 4): the five-port method was used. The subumbilical port was used for observation (12-mm trocar), the #1 robotic arm was placed on the left anterior axillary line under the costal arch (8-mm trocar), the #2 robotic arm was placed on the right anterior axillary line at the umbilical level (8-mm trocar), and the manual operative port was placed on the right mid clavicular line at 3 cm under the costal arch (12-mm trocar). An auxiliary port was placed on the left anterior axillary line at the umbilical level (8-mm trocar).
Thoracic ports (Figure 5): the five-port method was used. The observation port was placed on the right anterior axillary line at the 5th intercostal space (12-mm trocar), the #1 robotic arm was placed on right posterior axillary line at the 3th intercostal level (8-mm trocar), the #2 robotic arm was placed on the right posterior axillary line at 8th intercostal space (8-mm trocar), and the manual operative ports were placed on the right posterior axillary line at the 10th (5-mm trocar), and an axillary port were placed on the right anterior axillary line at 7th intercostal spaces (12-mm trocar).
Docking the robotic arms
The robotic arms were docked through the operation table overhead, the #1 robotic arm was connected to a bipolar electric coagulation forceps, and the #2 robotic arm was connected to a hook electrode. A lap-protector was used to avoid incision infection.
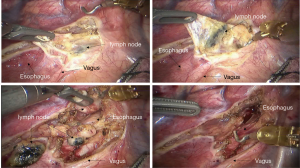
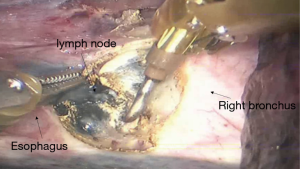
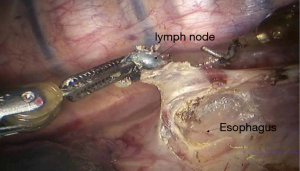
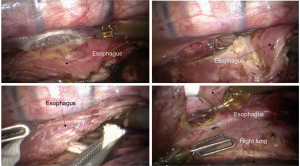
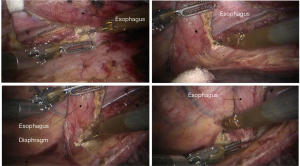
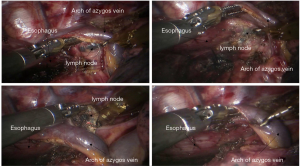
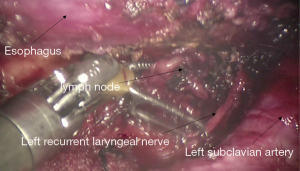
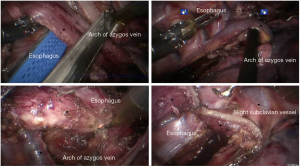
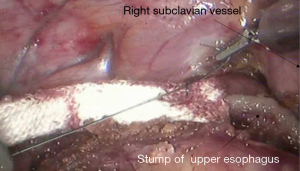
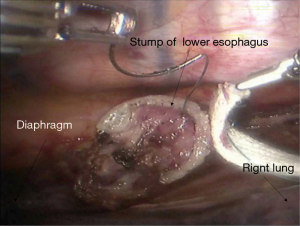
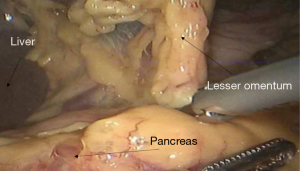
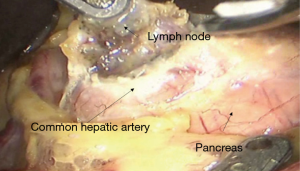
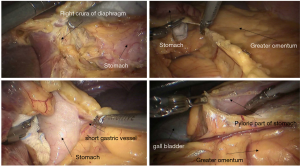
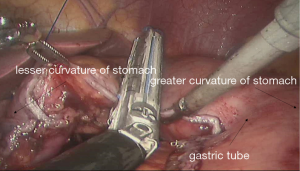
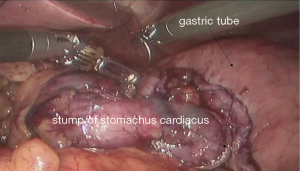
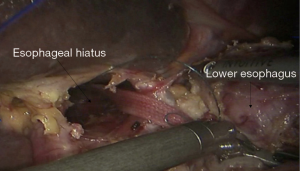
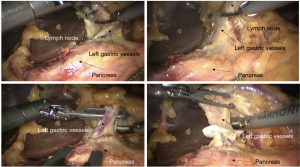
Surgical procedures
See Figures 6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23.
Postoperative results
The chest tube was removed on the second day postoperative day, and the patient was discharged on the sixth day postoperative day. No complications occurred during hospitalization. Pathologic diagnosis was esophageal squamous cancer (TNM stage was T3N0M0, stage IIA).
Comment
The first robotic-assisted minimally invasive esophagectomy (RAMIE) in the world was reported in 2003 by Dr. Horgan (1). Previously, research focused on RAMIE was limited because of the operative difficulties of minimally invasive esophagectomy, and the McKeown approach was the most widely adopted RAMIE approach. In 2010, Dr. Kim reported 21 cases of RAMIE to verify the feasibility and safety of the McKeown approach (2). In 2014, van der Sluis analyzed the clinical data of 108 patients who underwent RAMIE using the Mckeown approach. The results showed that in-hospital mortality was 5%, 5-year-survival was 42%, and 47.2% cases had local or systemic recurrences. In this case, to avoid potential local recurrence, we removed the tumor during the thoracic part of the operation and connected the stumps of the upper and lower esophagus by using ribbon gauze. We found that the three-dimensional vision and robotic arm provided great accessibility for the subtle manipulations, especially while dissecting lymph nodes around the recurrent laryngeal nerves. It was reported that RAMIE could reduce the incidence of hoarseness (3) and provide satisfactory short-term outcomes (4). However, whether RAMIE can provide long-term benefits to patients with esophageal cancer needs further study.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.01.18). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Horgan S, Berger RA, Elli EF, et al. Robotic-assisted minimally invasive transhiatal esophagectomy. Am Surg 2003;69:624-6. [PubMed]
- Kim DJ, Hyung WJ, Lee CY, et al. Thoracoscopic esophagectomy for esophageal cancer: feasibility and safety of robotic assistance in the prone position. J Thorac Cardiovasc Surg 2010;139:53-59.e1. [Crossref] [PubMed]
- Suda K, Ishida Y, Kawamura Y, et al. Robot-assisted thoracoscopic lymphadenectomy along the left recurrent laryngeal nerve for esophageal squamous cell carcinoma in the prone position: technical report and short-term outcomes. World J Surg 2012;36:1608-16. [Crossref] [PubMed]
- Han D, Xiang J, Gao T, et al. Robotic-assisted Versus Open Ivor-Lewis Esophagectomy for Esophageal Cancer: a Comparative Study on Short-term Results. Chin J Min Inv Surg 2016;16:404-7.
Cite this article as: Han D, Yang S, Guo W, Jin R, Zhang Y, Chen X, Wu H, Du H, Chen K, Xiang J, Li H. Robotic-assisted McKeown esophagectomy. AME Med J 2017;2:5.