Robot-assisted surgery for posterior superior mediastinal mass
Clinical data
Medical history
A 40-year-old woman was admitted to our hospital because of a posterior mediastinal mass. She had undergone a physical examination in a local hospital 1 month previously and received a diagnosis of a posterior mediastinal mass. One week previously she underwent a second contrast-enhanced computed tomography (CT) scan in our hospital, which showed a posterior mediastinal mass that measured 3.9 cm × 2.4 cm. She had no comorbidities such as diabetes, hypertension or heart disease.
Physical, laboratory and imaging examination
Physical examination
Body temperature was 36.8 °C. Heart rate was 92 beats per minutes. Respiratory rate was 20 breaths per minutes. Blood pressure was 130/78 mmHg. There was no positive sign detected during the physical examination.
Laboratory texts
Results of laboratory texts upon admission were negative.
Imaging examination
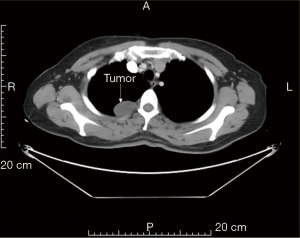
Chest contrast-enhanced CT (Figure 1): an oval soft-tissue density mass was found in the right posterior superior mediastinum. It measured 3.9 cm × 2.4 cm and had homogeneous density and smooth margin. No contrast-enhanced signal was found in the opacity.
Preoperative preparation
Conventional skin preparation and preoperative education were performed.
Procedures
Anesthesia and body position
The operation was conducted using general anesthesia. The patient was placed slightly forward in the left lateral recumbent position with single-lung ventilation. Conventional disinfection and draping were performed.
Incision ports
A 1.2 cm camera port was placed at the 5th intercostal space at the right mid-axillary line. Another two 0.8 cm utility ports were created. One of them was between the right posterior axillary line and the subscapular line, in the 8th intercostal space. The other one was at the 3th intercostal space between the anterior axillary line and midclavicular line.
Operation procedure
- The thoracic cavity was inspected and checked for pleural adhesion. An 8-mm artificial pneumothorax was established. The 1st robotic arm was connected to a unipolar cautery hook, and the 2nd robotic arm was connected to a bipolar cautery forceps. The mass and its relation to adjoining tissues and organs were inspected.
- The mediastinal pleura was opened and the tumor was dissociated along its edge.
- The tumor was completely resected.
- Hemostasis of the tumor bed was achieved.
- The dissected tumor was harvested.
- The thoracic cavity was lavaged and the errhysis was inspected.
- An indwelling drainage tube was placed in the camera port. The robot system was withdrawn. The chest was closed after sputum suction and lung recruitment. Total intraoperative blood loss was 5 mL.
Postoperative treatment
After the surgery, the patient received conventional adjuvant remedy. The drainage on postoperative day 1 was 20 mL. The patient was extubated on postoperative day 1. No postoperative morbidity was observed.
Pathologic diagnosis
Morphology: the mediastinal mass was 4 cm × 3 cm × 1.5 cm. The mass substance was moderately hard and looked like tofu. The pathologic diagnosis was mediastinal neurofibroma.
Commentary
For this patient, robotic thoracic surgery was safe and efficient. Compared with traditional video-assisted thoracoscopic surgery (VATS), the robotic system provides a clearer and more intuitive enhanced three-dimensional vision and seven degrees of freedom of the robotic arms (1). These advantages improved the ability to dissociate the mediastinal tumor and perform subtle dissection in a confined space. Furthermore, although the incision length is the same as that required for VATS, the robotic surgery caused less friction and injury to the intercostal nerve. It has been 14 years since Ichiro Yoshino conducted the first robotic-assisted extirpation of a posterior mediastinal mass in 2002 (2). Since then, additional studies have confirmed the feasibility, reliability, and superiority of this method (3-5). Furthermore, the learning curve of robotic thoracic surgery for a posterior mediastinal mass is quite short (4). However, to confirm the advantage of robotic surgery regarding postoperative and long-term survival, high-volume design, pain score, and use of postoperative anesthetic and long-term follow up is still needed.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.01.17). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Schmid T. Robotic Surgery Eur Surg 2002;3:155-7. [Crossref]
- Yoshino I, Hashizume M, Shimada M, et al. Video-assisted thoracoscopic extirpation of a posterior mediastinal mass using the da Vinci computer enhanced surgical system. Ann Thorac Surg 2002;74:1235-7. [Crossref] [PubMed]
- Bodner J, Wykypiel H, Greiner A, et al. Early experience with robot-assisted surgery for mediastinal masses. Ann Thorac Surg 2004;78:259-65; discussion 265-6. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Minnich DJ. Operative techniques in robotic thoracic surgery for inferior or posterior mediastinal pathology. J Thorac Cardiovasc Surg 2012;143:1138-43. [Crossref] [PubMed]
- Al-Mufarrej F, Margolis M, Tempesta B, et al. Novel thoracoscopic approach to difficult posterior mediastinal tumors. Gen Thorac Cardiovasc Surg 2010;58:636-9. [Crossref] [PubMed]
Cite this article as: Guo W, Yang S, Jin R, Zhang Y, Chen X, Wu H, Du H, Han D, Chen K, Xiang J, Li H. Robot-assisted surgery for posterior superior mediastinal mass. AME Med J 2017;2:10.