Collaboration between the surgeon, assistants and nurses in robotic-assisted thoracic surgery
Section 1: surgical instruments and preparation
Conventional surgical instruments
Routine surgical instruments: #7 knife handles, surgical scissors, forceps, needle holders, clamps (Snap, Kelly, Allis), Langenbeck, retractors, sponge-holding forceps, disinfection plates, and medicine bowls.
- Routine instruments for pulmonary surgeries (see Table 1).
Table 1
Routine instruments for pulmonary surgeriesEndoscopic instruments: 12-mm trocars, suction apparatus, pneumoperitoneum tubes, endoscopic forceps, scissors, 10mm titanium clips, Hem-o-lock clips, monopolar and bipolar energy instrument cord Disposable instruments: #22 blades, #11 blades, 9×24 needles, ruler, urethral catheterization bags, drainage pack, suction connecting tubes, electric scalpels, paraffin oil tampons, 6×7 and 10×10 wound dressings, imaging gauzes, imported rubber strips, Endo GIA autosuture single-use stapler and reloads, specimen fetcher, 32 Fr thoracic drainage tube, 8 Fr drainage tube, #0 5/8 VICRYL arc absorbable sutures, 3-0 fast absorbing skin sutures - Routine instruments for esophageal surgeries (see Table 2).
Table 2
Routine instruments for esophageal surgeriesEndoscopic instruments: 12-mm trocars, suction apparatus, pneumoperitoneum tubes, ultrasonic knife line, endoscopic forceps, scissors, 10-mm titanium clips, Hem-o-lok clips, monopolar and bipolar lines, endoscopic fan retractors, endoscopic double joint forceps, and endoscopic anvil- holding forceps Disposable instruments: #22 blades, #11 blades, 9×24 needles, ruler, urethral catheterization bags, drainage pack, suction connecting tubes, electric scalpels, protective sleeves, paraffin oil tampons, 6×7 and 10×10 wound dressings, imaging gauze 20 mL syringes, Endo GIATM autosuture single-use stapler and reloads, specimen fetcher, 32Fr thoracic drainage tube, 8Fr drainage tube, 200-mL negative pressure drainage bottle, jejunal fistula, 2-0 double-headed straight needles, 3-0 Prolene sutures, 3-0 MAXON sutures, 3-0 VICRYL absorbable sutures, #0 5/8 VICRYL arc absorbable sutures, 3-0 fast absorbing skin sutures
Other instruments needed for neck lymph nodes dissection: gauze, thyroid retractor, clamps (Mosquito, Snap), forceps, surgical scissors, 200-mL negative pressure drainage bottle, 3-0 sutures, and 6×14 round needles.
- Routine instruments for mediastinum and thymus surgeries (see Table 3).
Table 3
Routine instruments for mediastinum and thymus surgeriesEndoscopic instruments: 12-mm trocars, suction apparatus, pneumoperitoneum tubes, endoscopic forceps, scissors, 10-mm titanium clips, Hem-o-lok clips, monopolar and bipolar energy instrument cord Disposable instruments: #22 blades, #11 blades, 9×24 needles, ruler, urethral catheterization bags, drainage pack, suction connecting tubes, electric scalpel, paraffin oil tampons, 6×7 and 10×10 wound dressings, imaging gauze, specimen fetching device, 32 Fr thoracic drainage tube, #0 5/8 VICRYL arc absorbable sutures, 3-0 fast absorbing skin sutures
Instruments of the da Vinci surgical system
- Accessories: 8-mm trocar ×3, seal for trocar ×3, puncture device, collators for camera, adapters for camera and camera arm, light-transmitting instrument, sterile drapes for robotic arms and camera, and 30° lens (0° lens for mediastinal surgeries).
- Instruments: permanent cautery hook, fenestrated bipolar forceps, Cadiere forceps, Maryland bipolar forceps, large needle, monopolar curved scissors, and harmonic curved shears.
Other instruments
The operation table should be equipped with a nonadjustable hand shelf, a hand shelf with adjustable height and angle, two pelvic supports, foot supporter, fan-shaped instruments table, square-shaped instrument table, height-adjustable chair, surgical basin stand, cushions, elastic bandages, marker pens, and image recording apparatus.
Section 2: the layout of the operating rooms
The da Vinci Surgical System consists of several key components, including the follow: surgeon console, the patient-side cart, and the vision cart. Using the da Vinci Surgical System, the surgeon operates while seating at an ergonomically designed console a few feet from the patient, away from the aseptic area. The console is connected to the patient-side cart and the vision cart. The patient-side cart is the main instrument. The vision cart provides the surgical assistant with a broad perspective and visualization of the procedure. The vision cart should be placed near the operating table beyond the patient at an appropriate height and angle facing the surgical assistant. It is equipped with a lens, light source, and energy platforms and connected to the robotic arms through a monopolar or bipolar energy instrument cord. Placement of the patient-side cart should align the camera position, target area, and the central column of the patient-side cart. Place the patient-side cart in front of the patient’s head with arms 1 and 2 on the left side, and arm 3 at the back.
Place the anesthesia machine at the front left of the operating table to shorten the distance between the respiratory interface of the anesthesia machine and the tracheal intubation interface of the patient. Adjust the positions of the cords and fluid infusion pathway according to the position of the patient (left lateral or right-lateral). The anesthetist should be able to see both the monitor screen of the anesthesia machine and the vision system of the da Vinci system.
Section 3: the position of the patient
Patient position plays a key role in the success of the operation because of the difficulty in moving the patient-side cart during the operation. Unlike traditional open surgery, da Vinci surgery requires clear exposure of the incision and viscera and unlimited robotic arm movement in horizontal and vertical space. The optimal patient position varies according to the body type. Ensure normal physiological curvature without excessive traction of muscles and nerves. Protect the limbs of the patient to avoid postoperative complications due to compression.
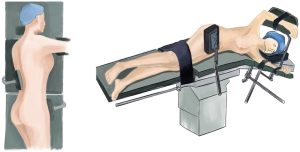
90° lateral position for pulmonary surgeries
Position the nonadjustable hand shelf at the level of the patient’s contralateral shoulder and then position the hand shelf with adjustable height and angle, which can maintain an unlimited operating field for the robotic arms and prevent the thorax from oppressing the upper limbs and brachial plexus (1). Move the patient to a 90° lateral position after giving anesthesia. A padded wedge or pillow is placed under the thorax at the level of the fourth and the fifth rib to bow the chest and open the rib spaces on the upper side to facilitate the exposure. Place the patient’s waist facing the back plate of the operation table to avoid disturbance of the pelvis by the robotic arms during surgery (Figure 1). Place the ipsilateral upper limb on the adjustable hand shelf angled outwards to 15°-20°, and the contralateral upper limb on the unadjustable hand shelf. Use elastic bandages and restraint straps to fix the upper limbs from the distal side to proximal side with appropriate pressure and expose the fingers to observe the peripheral circulation. The lateral position is maintained by pelvic and buttock supports which prevent rolling or slipping. The upper leg is placed in a flexed position, and the lower leg in an extended position. Cushions are placed not only between the legs, but also under the knees and ankles. Use restraint straps to fix the lower limbs.
90° lateral position and supine position for esophageal surgeries
The 90° lateral position used for esophageal surgeries is almost the same as the 90° lateral position used for pulmonary surgeries. Place the patient slightly forward and maintain the 15° reverse Trendelenburg position to provide excellent exposure for the surgeon (Figure 2).
The supine position for esophageal surgeries
With the patient in a supine position, add a bedside board for neck lymph node dissection. Place a cushion under the thorax and the waist to prevent post-operative discomfort. Place a cushion under the knee joint to ensure normal physiological curvature. Place a cushion under the heel to prevent compression. Fix restraint straps above the knee joint with appropriate tightness. Place the patient’s left arm (used for intravenous injection) on the hand shelf angled outwards less than 90° and fix with a restraint strap. Fix the other arm using the same approach with good protection. Use a foot supporter to prevent slipping. Maintain a 10°-15° reverse Trendelenburg position and tilt the operation table 10°-15° to the right to better expose the stomach (Figure 2).
Place the patient in the supine Trendelenburg position for neck lymph nodes dissection. Place occiput supports under the cervical vertebrae to avoid excessive neck traction (Figure 3).
Position for mediastinal surgeries
Mediastinal surgeries can be divided into anterior mediastinal surgeries and posterior mediastinal surgeries. Anterior mediastinal surgeries require the patient to be in a 45° semi-lateral position with the patient-side cart at the contralateral side. Posterior mediastinal surgeries require the patient to be in a 90° lateral position with the patient-side cart at the ipsilateral side.
For the 45° semi-lateral position, place the contralateral arm on the hand shelf angled outwards to less than 90°. Place pelvic supports at the axilla and iliac crest to prevent movement when the table is rolled. Place slope-shaped cushions under the ipsilateral shoulder and hip, and place a cushion under the waist. The patient’s upper body should be in a 45° semi-lateral position. Use a cotton pad to protect the ipsilateral wrist and fix it to the operation table with an elastic bandage to avoid excessive traction and compression. Place a cushion under the knee joint and use a foot supporter. Fix the lower limbs (Figure 2).
The 90° lateral position for posterior mediastinal surgeries is nearly the same as the 90° lateral position for pulmonary surgeries. Tilt the operation table 10° to the ipsilateral side for better exposure.
Section 4: intraoperative collaboration
Patient protection and the use of protective equipment
The patient is often placed in the lateral position after receiving anesthesia in thoracic surgeries. The anesthetists and nurses should cooperate to avoid tracheal intubation or infusion tube slipping because of the traction due to inappropriate posture. Muscle relaxation caused by anesthesia makes the limbs vulnerable to hyperextension or compression, especially in certain position that allow exposure of the surgical field. Protective equipment for patient position include a silicone bedsore pad, heel pad, cushions, cotton pad, foot supporter, elastic bandages, elastic restraint straps, hand shelf with adjustable height and angle, and iliac supporter.
Preparation for special surgical dressings and sutures
Because of the magnified view of the operative field in da Vinci robotic surgeries, it is suitable to use compact gauze (length 5 cm, diameter 7–8 mm) made by nurses, which have a smooth surface without protruding threads to facilitate the absorption of exudates and blood in the surgical field.
The sutures used in robotic surgeries should be 8 cm for interrupted sutures, 18–20 cm for continuous sutures, and original length for purse-string sutures and with strict sterilization.
Choice of single-use staplers and reloads
Use Endo GIATM 60-3.5 reloads to cut the pulmonary lobe, 60-4.8 reloads to cut the bronchus and 60-2.5/45-2.5/30-2.5 reloads to cut the pulmonary blood vessels in pulmonary surgeries.
Use Endo GIATM 60-3.5 reloads and 60-3.5 rotatable reload to make the gastric tube in esophageal surgeries. Use 60-2.5 reloads for the arch of azygos vein.
Section 5: cooperation between surgical team members and problem solving in robotic thoracic surgeries
Teamwork
The surgical team members in robotic thoracic surgeries include the surgeon, surgical assistant, anesthetist, instrument nurses, and circulating nurses. The surgical team should have clearly defined roles and cooperate well. Double-lumen endotracheal intubation, stable ventilation, and hemodynamics are important prerequisites to ensure a smooth operation. Instrument nurses should be familiar with the use of robotic arms and sterile drapes for robotic arms, lens settings, loading and firing of the special instruments in the da Vinci system, and the surgical procedure. Circulating nurses should make the preparations for da Vinci robotic surgery including setting up the system, self-checking, robotic arms, and lens loading. They should move the patient-side cart to the appropriate position beside the operation table to facilitate the connections between robotic arms and the trocars. Circulating nurses also need to help position the patient and observe and protect the patient during surgery.
Problem solving
Clear endoscopic operative view
The lens of the da Vinci system provides the surgeon with two visual fields, whereas the vision cart only shows only one visual field. If the visual field is obscured due to exudation or fog generated by electric scalpels, the surgical assistant should take out the lens and use wet gauze to scrub the lens and trocar to prevent blood from the clouding the lens again. Readjust the focus.
Instrument changing and error solving
The surgeon should instruct the surgical team to change the robotic arms and straighten the wrist of the robotic arm when it is open slightly. The instrument nurse should confirm this with the surgeon before removing the robotic arms. It is important to use the instruments appropriately. Effective communication is the key to avoiding unnecessary injury to the patient, maintaining normal operation of the da Vinci system, and shortening the surgery time.
The circulating nurse should be able to deal with system alarms and errors. Common problems such as power connection issues or crash of the robotic arms could be handled with the clutch. Reinsert or change the robotic arm and use the recovery button in the event of a system alarm. Record the fault code and inform the engineer in the event of an unrecoverable fault.
The surgical assistant and nurses should ask the surgeon to pause the surgery and change the position of the robotic arms if there is robotic arms crash. Be sure to protect the incisions.
Emergency coordination for conversion to open surgery
Promptly prepare the instruments for open surgery (e.g., headlamp, electric scalpels, and ultrasonic knives, if needed) under the instruction of the surgeon and remove the da Vinci surgical instruments to provide enough space for open surgery (Table 4). Adjust the operation table to the appropriate height and angle for open surgery and protect and restrict the patient’s limbs. Avoid unnecessary exposure of the limbs and use an electric blanket to maintain the patient’s body temperature.
Table 4
| Routine instruments: routine thoracic instruments for open pulmonary surgeries, retractors (auto-retractors for small incisions or crossed retractors), handles for shadowless lamp, measuring cylinder and special instruments for esophageal surgery |
| Disposable instruments: Yankauer suction tip, extension for electric scalpels, trocars, 2-0 sutures, 0 sutures, 3-0 Prolene sutures, 4-0 Prolene sutures, 5-0 Prolene sutures, ultrasonic knives, gauze, 20 or 25 cm wound dressings, and spherical irrigator |
Acknowledgements
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, AME Medical Journal. The article did not undergo external peer review.
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.01.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang S. The Robotic Thoracic Surgery. China: AME Publishing Company, 2015.
Cite this article as: Li J, Wang W, Qian Q, Chen X, Li H. Collaboration between the surgeon, assistants and nurses in robotic-assisted thoracic surgery. AME Med J 2017;2:21.