
The Feasibility of cortical bone trajectory screw fixation for lower thoracic spine
The traditional pedicle screw fixation technique is described widely used in cervical, thoracic, lumbar, and sacral regions (1,2), which can provide strength biomechanical properties for most spinal surgery. However, there are some drawbacks of traditional pedicle screw fixation. The trajectory is from lateral to medial, and the screw entry point is located on the cross of middle horizon line of transverse process and the middle vertical line or lateral wall of the upper facet (3,4). Therefore, surgeons need considerable paraspinal muscle dissection for traditional pedicle screw fixation.
Additionally, traditional pedicle screw has high risk of screw loose for osteoporotic patients (5). Several alternative techniques were developed to increase the pullout force of traditional pedicle screw fixation for osteoporotic patients, including using screw with lager diameter and bone cement augmentation (6).
Santoni et al. (7) firstly reported lumbar cortical bone trajectory (CBT) screw fixation technique, which is from middle to lateral direction in axial plane and caudocephalad direction in the sagittal plane. Compared to the traditional pedicle screw fixation, CBT screw is shorter and smaller, with the maximized thread to contact with the higher density cortical bone, and not penetrating the vertebral body trabecular bone (8).
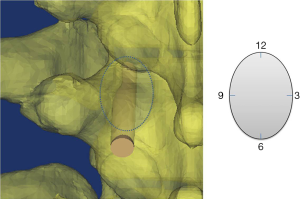
There are many studies that proved the morphometric feasibility and biochemical properties of CBT screw fixation in the lumbar spine region (7,9,10), and some clinical studies to investigate the outcomes of this technique in treatment of patients with lumbar spine pathologies (11-13). In lower thoracic spine region (T9–T12), it is Matsukawa et al. that firstly reported (14) the morphometric measurements and feasibility of CBT screw fixation technique on 50 adults’ CT scans. The point of intersection of the lateral two thirds of the superior articular process and the inferior border of the transverse process was used as the screw entry point. Then, the CBT trajectory was designed straight forward in the axial plane angulated cranially targeting the posterior third of the superior endplate (6 o’clock orientation and aimed in the 12 o’clock direction in the pedicle) (Figure 1). After the CT images measured, 24 cadaveric thoracic vertebrae (5 T9, 5 T10, 6 T11, and 6 T12, with 44 pedicles) were further studied.
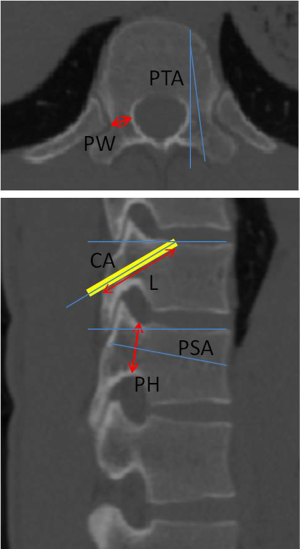
In CT morphometric measurements of T9–T12 region, parameters were measured (Figure 2): (I) pedicle width (PW); (II) pedicle height (PH); (III) pedicle transverse angle (PTA); (IV) pedicle sagittal angle (PSA); (V) length of screw trajectory (L); (VI) cephalad angle (CA). They found that the PW gradually increased from T9 (6.0±1.1 mm) to T12 (9.1±1.6 mm); the PH gradually increased from T9 (13.0±1.3 mm) to T12 (16.8±1.7 mm); while the transverse and sagittal angles of the pedicle tended to decrease gradually from T9 (7.7±1.9° and 14.9±3.4°) to T12 (4.4±1.71° and 10.4±3.1°). The length of trajectory was from 29.7±4.6 mm (T9) to 32.0±2.1 mm (T12), and the CA from 21.4±3.3° (T9) to 27.6±3.9° (T12).
Then, they compared the maximum insertional torques of CBT screw fixation and the traditional pedicle screw fixation on 24 lower thoracic vertebrae, and found that CBT screw (diameter: 5.5 mm; length: 35 mm) had the maximum insertional torque of 1.02±0.25 Nm, which is significantly better than the traditional pedicle screw (diameter: 6.0 mm; length: 40 mm) of 0.66±0.15 Nm.
This study proved the feasibility of CBT screw fixation in lower thoracic region, and gave us amount of valuable data to guide the clinical performance. However, there were still some problems, the PW of T9 was 6.0±1.1 mm, this means lots of patients had the PW less than 5.5 mm, Zhuang et al. (15) reported that the percentage of PW lesser than 4.5 mm is 34.75% at T9 in female population, and 40.91% in female who is less than 160 cm. Therefore, the screw with diameter of 5.5 mm may penetrate out the cortical bone. The other caution need to take is that the lamina width of T12 is very small, which may have high risk of lateral pars fractures.
Xuan et al. (16) reported to insert the 4.5 mm diameter CBT screws via pedicle or pedicle rib unit in lower thoracic spine. They found the 4.5 mm diameter CBT screws can be placed at T11 and T12 via pedicle only, but need via pedicle rib unit at T9 and T10 in some patients because the screw penetrated the outer wall of pedicle cortex, especially in females. They (17) also provided the anatomic data of performing 4.5 to 5.5 mm CBT screws fixation via pedicle or pedicle rib unit in the pediatric thoracic spine. The above two studies add the additional evidence and novel concept to CBT screws fixation in lower thoracic spine to Matsukawa et al. (14).
The aim of using CBT screw fixation is to improve the stability and pullout strength. Matsukawa et al. (14) only reported the insertional torque, further biomechanical tests including cyclic moments (flexion/extension/lateral bending/axial rotation) loading test in six freedom machine, fatigue test and pullout test of CBT screw in lower thoracic spine need to be conducted. Moreover, the clinical studies should also be conducted further to prove its safety and efficacy.
Acknowledgements
Funding: This work was funded by the National Natural Science Foundation of China (81501933, 81371988), Wenzhou Municipal Science and Technology Bureau (Y20170369).
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, AME Medical Journal. The article did not undergo external peer review.
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.08.09). Dr. Wu serves as an unpaid section editor of AME Medical Journal. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kabins MB, Weinstein JN. The History of Vertebral Screw and Pedicle Screw Fixation. Iowa Orthop J 1991;11:127-36.
- Wu AM, Zou F, Cao Y, et al. Lumbar spinal stenosis: an update on the epidemiology, diagnosis and treatment. AME Med J 2017;2:63. [Crossref]
- Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res 1986;7-17. [PubMed]
- Inceoğlu S, Montgomery WH Jr, St Clair S, et al. Pedicle screw insertion angle and pullout strength: comparison of 2 proposed strategies. J Neurosurg Spine 2011;14:670-6. [Crossref] [PubMed]
- Wittenberg RH, Shea M, Swartz DE, et al. Importance of bone mineral density in instrumented spine fusions. Spine (Phila Pa 1976) 1991;16:647-52. [Crossref] [PubMed]
- Wittenberg RH, Lee KS, Shea M, et al. Effect of screw diameter, insertion technique, and bone cement augmentation of pedicular screw fixation strength. Clin Orthop Relat Res 1993;278-87. [PubMed]
- Santoni BG, Hynes RA, McGilvray KC, et al. Cortical bone trajectory for lumbar pedicle screws. Spine J 2009;9:366-73. [Crossref] [PubMed]
- Phan K, Hogan J, Maharaj M, et al. Cortical Bone Trajectory for Lumbar Pedicle Screw Placement: A Review of Published Reports. Orthop Surg 2015;7:213-21. [Crossref] [PubMed]
- Matsukawa K, Yato Y, Nemoto O, et al. Morphometric measurement of cortical bone trajectory for lumbar pedicle screw insertion using computed tomography. J Spinal Disord Tech 2013;26:E248-53. [Crossref] [PubMed]
- Calvert GC, Lawrence BD, Abtahi AM, et al. Cortical screws used to rescue failed lumbar pedicle screw construct: a biomechanical analysis. J Neurosurg Spine 2015;22:166-72. [Crossref] [PubMed]
- Iwatsuki K, Yoshimine T, Ohnishi Y, et al. Isthmus-guided cortical bone trajectory for pedicle screw insertion. Orthop Surg 2014;6:244-8. [Crossref] [PubMed]
- Takata Y, Matsuura T, Higashino K, et al. Hybrid technique of cortical bone trajectory and pedicle screwing for minimally invasive spine reconstruction surgery: a technical note. J Med Invest 2014;61:388-92. [Crossref] [PubMed]
- Rodriguez A, Neal MT, Liu A, et al. Novel placement of cortical bone trajectory screws in previously instrumented pedicles for adjacent-segment lumbar disease using CT image-guided navigation. Neurosurg Focus 2014;36:E9. [Crossref] [PubMed]
- Matsukawa K, Yato Y, Hynes RA, et al. Cortical Bone Trajectory for Thoracic Pedicle Screws: A Technical Note. Clin Spine Surg 2017;30:E497-E504. [PubMed]
- Zhuang Z, Chen Y, Han H, et al. Thoracic pedicle morphometry in different body height population: a three-dimensional study using reformatted computed tomography. Spine (Phila Pa 1976) 2011;36:E1547-54. [Crossref] [PubMed]
- Xuan J, Zhang D, Jin HM, et al. Minimally invasive cortical bone trajectory screws placement via pedicle or pedicle rib unit in the lower thoracic spine: a cadaveric and radiographic study. Eur Spine J 2016;25:4199-207. [Crossref] [PubMed]
- Xuan J, Chen J, He H, et al. Cortical bone trajectory screws placement via pedicle or pedicle rib unit in the pediatric thoracic spine (T9-T12): A 2-dimensional multiplanar reconstruction study using computed tomography. Medicine (Baltimore) 2017;96:e5852. [Crossref] [PubMed]
Cite this article as: Chen D, Ni WF, Lin Y, Wang XY, Wu AM. The Feasibility of cortical bone trajectory screw fixation for lower thoracic spine. AME Med J 2017;2:123.

