Efficacy and safety of integration of traditional and Western medicine for the treatment of spontaneous bacterial peritonitis in liver cirrhosis: a systematic review
Background
Liver cirrhosis is the end stage of liver diseases with a high morbidity and mortality (1). Ascites is the most common complication of liver cirrhosis. Nearly 60% of patients diagnosed with liver cirrhosis will develop ascites within 10 years (2). Spontaneous bacterial peritonitis (SBP) is a common bacterial infection in cirrhotic patients with ascites. The morbidity and in-hospital mortality of SBP in patients with ascites is 7–30% and 10–50% (3-5).
Several guidelines unanimously recommend third-generation cephalosporins for the treatment of SBP (6-8). However, antibiotic resistance is increasing year by year in SBP patients (9-11). The effectiveness of antibiotics alone for the treatment of SBP is unsatisfactory.
Traditional Chinese medicine (TCM) refers to the drugs and compounds used under the guidance of the TCM theory. Integration of traditional and Western medicine (ITWM) refers to the combination of TCM with Western medicine, which has a great potential for the treatment of many diseases in China (12-14). More and more studies have focused on the ITWM for the treatment of SBP in China.
The aim of this study was to systematically evaluate the efficacy and safety of ITWM for the treatment of SBP.
Materials and methods
Eligibility and exclusion criteria
Eligibility criteria: randomized controlled trials (RCTs) about ITWM for the treatment of SBP in patients with cirrhosis. ITWM group should be patients who received TCM drugs combined with Western medicine drugs. Control group should be patients who received Western medicine drugs alone. Exclusion criteria: (I) incomplete data; (II) reviews; (III) case reports; (IV) duplicate publications; (V) commentaries; (VI) non-RCTs; and (VII) ITWM in the prevention of SBP. No limits on publication status or language.
Literature search
PubMed, China National Knowledge Infrastructure, Wanfang, and VIP databases were searched electronically from inception to July 2016 to collect all RCTs about ITWM for the treatment of SBP in patients with liver cirrhosis. All databases were searched using key words: TCM, SBP, and ITWM.
Data extraction
Data were extracted as follows: title, author’s information, year of publication, study design, method of intervention, effectiveness of treatment, and adverse event.
Effectiveness rate was defined as the proportion of patients in whom SBP-related symptoms and/or laboratory data improved after treatment.
Cure rate was defined as the proportion of patients in whom SBP-related symptoms disappeared and laboratory data normalized after treatment.
Ineffectiveness rate was defined as the proportion of patients without any response to treatment.
Quality of studies
Jadad quality score was used to assess the quality of studies (Table S1) (15).
Randomization: studies using the method of randomization appropriately were graded as 2 points; studies without any description about the method of randomization were graded as 1 point; studies using the method of randomization inappropriately were graded as 0 point.
Double blinding: studies using and describing the double blinding method appropriately were graded as 2 points; studies in which the use of double blinding was just mentioned but the detailed method was lacking were graded as 1 point; studies in which the double blinding method was not used or the method of double blinding was inappropriate were graded as 0 point.
Withdraws and dropouts: studies in which both withdraws and dropouts were described were graded as 1 point; studies in which withdraws and dropouts were not described were graded as 0 point.
Results
Basic information
A total 628 studies were identified. Finally, 42 RCTs including 3,227 SBP patients were enrolled into this study (Figure 1). Information of the included studies is depicted in the Table S2. The distributions of included studies according to the region of China are described in the Figure S1.
Medications
Components of TCM-drugs
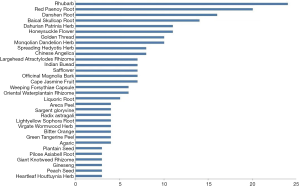
The most commonly used TCM drugs were demonstrated in Figure 2. Overall, 77 kinds of TCM drugs were used, including Rhubarb (N=24), Red Peony Root (N=20), Danshen Root (N=16), Baical Skullcap Root (N=14), Dahurian Patrinia Herb (N=11), Honeysuckle Flower (N=11), Golden Thread (N=10), Mongolian Dandelion Herb (N=10), Spreading Hedyotis Herb (N=8), Chinese Angelica (N=8), Largehead Atractylodes Rhizome (N=7), Indian Buead (N=7), Safflower (N=7), Officinal Magnolia Bark (N=7), Cape Jasmine Fruit (N=7), Weeping Forsythiae Capsule (N=6), Oriental Waterplantain Rhizome (N=6), Liquoric Root (N=5), Areca Peel (N=4), Sargent Gloryvine (N=4), Radix Astragali (N=4), Lightyellow Sophora Root (N=4), Virgate Wormwood Herb (N=4), Bitter Orange (N=4), Green Tangerine Peel (N=4), Agaric (N=4), Plantain Seed (N=3), Pilose Asiabell Root (N=3), Giant Knotweed Rhizome (N=3), Ginseng (N=3), Peach Seed (N=3), Heartleaf Houttuynia Herb (N=3), Indigowoad Root (N=2), Turtle Shell (N=2), Tangerine Peel (N=2), Myrrh (N=2), Frankincense (N=2), Common Yam Rhizome (N=2), Yanhusuo (N=2), Coix Seed (N=2), Turmeric Root-tuber (N=2), Hiraute Shiny Bugleweed Herb (N=2), Medicinal Indianmulberry Root (N=1), White Hyacinth Bean (N=1), Chinese Pulsatilla Root (N=1), Barbed Skullcap Herb (N=1), Pinellia Tuber (N=1), Areca Seed (N=1), Borneol (N=1), Chinese Thorowax Root (N=1), Halloysit (N=1), Rice Bean (N=1), Common Andrographis Herb (N=1), Indigowoad Leaf (N=1), Zedoary (N=1), Turmeric (N=1), Platycodon Root (N=1), Semen Nelumbinis (N=1), Beautiful Sweetgum Fruit (N=1), European Verbena (N=1), Parslane Herb (N=1), Dwarf Lilyturf Tuber (N=1), Mirabilite (N=1), Oyster Shell (N=1), Bezoar (N=1), Goat Horn (N=1), Common Clubmoss Herb (N=1), Garden Balsam Stem (N=1), Ground Beeltle (N=1), Cowherb Seed (N=1), Bear Gall Powder (N=1), Figwort Root (N=1), Dragon’s Blood (N=1), Motherwort Herb (N=1), Epimedium Herb (N=1), Pearl Powder (N=1), and Common Anemarrhena Rhizome (N=1).
There were 12 categories of TCM drugs, including formula for heat-clearing and toxicity-relieving (N=20), formula for blood circulation promoting (N=13), formula for energy-restoring (N=12), formula for water-disinhibiting damp-percolating (N=8), desiccating formula (N=4), carminative formula (N=4), astringent formula (N=3), superficies-resolving formula (N=2), formula for purgation (N=2), formula for rheumatism (N=2), formula for expectorants, antitussives and dyspnea-relieving (N=2), and formula for resuscitation (N=1).
Western medicine drugs
The third-generation cephalosporins, including cefoperazone and ceftriaxone, were the most commonly used Western medicine drugs for the treatment of SBP (71.43%, 30/42).
Form of TCM drugs
Of all included studies, 38.10% (16/42) used the TCM decoction (16-31), 28.57% (12/42) used the Chinese patent medicine (32-43), 21.43% (9/42) used the TCM enema (44-51), 9.52% (4/42) used the TCM umbilicus compression (52-55), and 2.38% (1/42) used the TCM peritoneal lavage (56).
Of all included studies, 4.76% (2/42) used the single-TCM drug (27,57), 30.95% (13/42) used the TCM compounds that have been proven by the China Food and Drug Administration (CFDA) (22,32-43), 16.67% (7/42) used the classical TCM compounds (16-19,25,31,54), and 47.62% (20/42) used the self-made TCM compounds (20,21,23,24,26,28-30,44-53,55,56).
Effectiveness rate
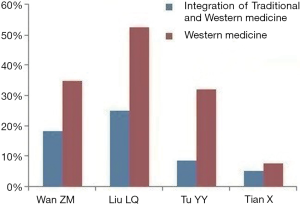
All included studies reported the effectiveness rate. The effectiveness rate was 58.33–96.00% and 32.20–93.75% in ITWM and control groups, respectively (Figure 3). Of all included studies, 97.62% (41/42) reported a higher effectiveness rate in ITWM group; and 92.69% (38/41) of them found a significant difference.
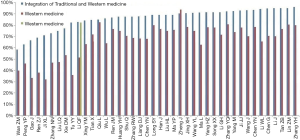
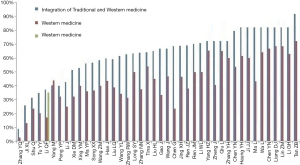
Cure rate
All included studies reported the cure rate. The cure rate was 9.00–95.00% and 3.00–77.00% in ITWM and control groups, respectively (Figure 4). Of all included studies, 97.62% (41/42) reported a higher cure rate in ITWM group and 24.39% (10/41) of them found a significant difference.
In-hospital mortality
Four studies reported the in-hospital mortality. The in-hospital mortality was 5.10–18.33% and 7.69–52.78% in ITWM and control groups, respectively (Figure 5). All of the four included studies reported a lower in-hospital mortality in ITWM group; and 50% (2/4) of them found a significant difference.
Adverse events
Six studies reported the adverse events, including abdominal pain, diarrhea, vomiting, headache, and rash. The rate of adverse events was 0.00–13.33% and 0.00–59.52% in ITWM and control groups, respectively (Figure 6). Five of them (83.33%, 5/6) reported a lower rate of adverse events in ITWM group; and 80% (4/5) of them found a significant difference.
Study quality
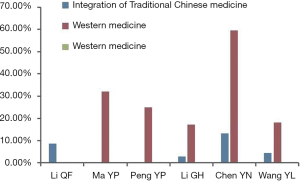
Of all included studies, 30.95% (13/42) didn’t describe any method of randomization; 64.29% (27/42) used the randomization but didn’t describe any method of randomization; and 4.76% (2/42) used the random number table (Table S1). No studies used the double-blind method. No studies reported the withdrawal/dropout rates.
Discussion
TCM drugs have been used for the treatment of many diseases for over 2,000 years in China and Eastern Asian countries (58). TCM theory is based on the ancient Chinese philosophy, aiming to correct the maladjustments, restore the self-regulatory ability, and remove the harms (59). Due to the language barrier, studies that reported the effectiveness of ITWM for the treatment of SBP are rarely noticed in the Western world. As far as we concern, no review explored the ITWM for the treatment of SBP. Our systematic review found the following: 92.69% (38/41) and 24.39% (10/41) of included studies reported a significantly higher effectiveness and cure rate in ITWM group, respectively; 50% (2/4) showed a significantly lower in-hospital mortality in ITWM group; and 66.67% (4/6) showed a significantly lower proportion of adverse events in ITWM group. Thus, ITWM should be a promising treatment for SBP. Additional benefits of ITWM might be attributed to the inhibition of inflammation, improvement of immunity, regulation of intestinal microflora, improvement of antibiotics bioavailability, and inhibition of drug resistance. However, the accurate mechanisms remained unclear.
Our study also showed that Rhubarb was the most commonly used TCM drug, followed by Red Paeony Root and Danshen root. First, Rhubarb was used in 57.14% (24/42) of studies, which has a role in defecation-accelerating, heat-clearing, blood-cooling, toxin-relieving, blood stasis-dredging, dampness-dredging, and jaundice-resolving according to the TCM theory. Modern pharmacological studies conclude that Rhubarb can protect the digestive tract mucosa and promote the gastrointestinal peristalsis (60). Second, Red Paeony Root was used in 83.33% (20/42) of studies. The dry root of Paeonia Lactiflora Pallas has a role in heat-clearing, blood-cooling, toxin-relieving, and blood stasis-dredging according to the TCM theory. Third, Danshen root was used in 38.10% (16/42) of studies, which has a role in blood circulation-promoting, blood stasis-dredging, and blood-nourishing according to the TCM theory. Anti-inflammatory functions of Red Paeony Root and Danshen Root have been proved (61,62). Additionally, both Red Paeony Root and Danshen Root are the main components of Xuebijing injection, which is the ethanol extract derived from Chuanxiong, Red Paeony Root, Danshen Root, and Honghua. It is the most commonly used Chinese herb compound in all included studies, well-known by its anti-inflammatory function (63). Seven (16.67%) studies used Xuebijing injection for the treatment of SBP.
There are many different forms of TCM drugs, including decoction, enema, sticking, and compound injection. Decoction is the most commonly used form of TCM drugs. It has some advantages: (I) the composition of a decoction can be modified according to the patient’s condition; (II) water is the main carrier to promote the absorption of TCM drugs; and (III) TCM decoction is widely used in China and becomes more and more popular worldwide. However, it also has some disadvantages: (I) TCM decoction is a complex composition that is composed by different TCM drugs. However, the interaction among TCM drugs after boiling and taking remains unclear; (II) the process of preparing a TCM decoction is complex; (III) the quality of TCM drugs after decocted is variable; and (IV) TCM compounds are highly individualized, the indications for modifying the TCM drugs or compounds are unclear.
Safety of ITWM treatment should be carefully evaluated. However, adverse events related to ITWM treatment were generally lacking. Non-specific adverse events (including abdominal pain, diarrhea, vomiting, headache, and rash) were only reported in six studies. No study described the risk factors, management, and outcome of adverse events. Thus, in future studies, there is a need for more detailed reporting on this matter. Additionally, some TCM drugs, such as Medicinal Indian Mulberry Root and Yanhusuo, have the potential of inducing liver and/or renal injury (64,65). Thus, they might be cautiously used in patients with liver and/or renal diseases. Notably, our systematic review demonstrated neither liver nor kidney toxicity of Medicinal Indian Mulberry Root and Yanhusuo.
We found that 30.95% of studies used the CFDA-proved TCM compounds, 16.67% of studies used the classical TCM compounds, and 47.62% of studies used the self-made TCM compounds. The CFDA-proved TCM compounds can be identified on the CFDA official website (http://www.sda.gov.cn/WS01/CL0001/). The classical TCM compounds can be identified from the classic books of TCM and are recognized by many TCM practitioners. The self-made TCM compounds are invented by some TCM practitioners based on their own clinical experiences. Certainly, the quality of the self-made TCM compounds may be uncertain. Only two studies (27,57) used the single-TCM drug (Rhubarb and Heartleaf Houttuynia Herb).
Some limitations should be pointed out. First, the ITWM treatment strategy and patients’ conditions are different among studies, which cause different rates of effectiveness, cure, and adverse events among studies. Thus, the data was not pooled due to these huge heterogeneities among studies. Second, a uniform definition of “therapeutic effectiveness” was lacking, which might contribute to the heterogeneity. For example, in Zhang’s paper, the definition of “effectiveness” was broad and easy to achieve, but the definition of “cure” was strict (36). This may lead to a higher effectiveness rate and a lower cure rate. Third, the quality of included studies was relatively poor. The quality of TCM RCTs performed in China has been questioned (66). Almost all TCM RCTs claimed a superiority of TCM treatment, but only few of them were of high-quality. Some methodological components of the RCTs were incompletely reported. Wang et al. (67) identified a total of 7,422 RCTs published between 1999 and 2004. Surprisingly, only 17.9% (1,329/7,422) of them were truly randomized. Forth, the risk control of TCM drugs was unavailable (68). Fifth, there are few TCM specialized hospitals in Western countries. Thus, the TCM RCTs were hardly performed in Western countries. It is also hard to extrapolate our conclusions to Western countries. Sixth, only 11 out of the 42 trials used albumin for the SBP treatment. Indeed, the lack of albumin administration in most of the trials included is a reason of concern, because it impairs the subjects’ outcome and makes difficult to compare the results.
In conclusion, ITWM might be effective and safe for the treatment of SBP. However, the quality of studies on ITWM for the treatment of SBP should be improved in future. Further well-randomized, double-blind, and placebo-controlled studies with a strict and uniform definition of effectiveness (i.e., partial response) and cure (i.e., complete response) are needed to explore the benefit/risk of a specific TCM drug or compound (i.e., Rhubarb or Xuebijing injection) for the treatment of SBP.

Table S1
| Author | Jadad scores |
|---|---|
| Li QF | 1 |
| Chen YN | 1 |
| Chen YN | 1 |
| Ren ZJ | 1 |
| Long SY | 1 |
| Yang HZ | 0 |
| Huang YH | 0 |
| Xie DM | 1 |
| Li J | 1 |
| Li WL | 1 |
| Qiu L | 0 |
| Ren JM | 1 |
| Liang DJ | 0 |
| Lin ZM | 0 |
| Chen G | 1 |
| Wan ZM | 1 |
| Gao J | 1 |
| Liu LQ | 1 |
| Tu YY | 0 |
| Wu L | 0 |
| Han J | 1 |
| Tian X | 1 |
| Xing YM | 1 |
| Ji XL | 1 |
| Liu HL | 1 |
| Jing XH | 1 |
| Ma YP | 1 |
| Li GH | 0 |
| Yang M | 1 |
| Peng YP | 0 |
| Ji JJ | 0 |
| Zhang YH | 0 |
| Song XX | 1 |
| Tan ZB | 1 |
| Zhang YQ | 1 |
| Wang J | 1 |
| Shu Q | 1 |
| Zheng J | 0 |
| Zhang RW | 2 |
| Wang YL | 1 |
| Ma L | 0 |
| Zhang NN | 2 |
Table S2
| First author [year] | Strategy of the treatment | No. patients | Effectiveness rate (%) | Cure rate (%) | Ineffectiveness rate (%) | Mortality (%) |
|---|---|---|---|---|---|---|
| LI QF (16) [1995]# | ITWM treatment | |||||
| Taking TCM decoction: DaChengQi Decoction add or subtract TCM drugs with the clinical symptoms, 1-time/day, for 7 days | 35 | 82.9 | 37.14 | 17.1 | NA | |
| Antibiotics: Norfloxacin 0.6 g, 3-time/day, taken orally for 10 days | ||||||
| Western medicine treatment | ||||||
| Norfloxacin 0.6 g, 3-time/day, taken orally for 10 days | 35 | 51.4 | 17.14 | 48.6 | NA | |
| Cefazolin 2.0 g, 2-time/day, for 10 days | 34 | 82.4 | 35.29 | 17.6 | NA | |
| Chen YN (17) [1997]# | ITWM treatment | |||||
| Taking TCM decoction: SanHuangXiaoDu Decoction: Spreading Hedyotis Herb 60 g, Baical Skullcap Root, Golden Thread, Rhubarb, Cape Jasmine Fruit 12 g, respectively; Honeysuckle Flower, Mongolian Dandelion Herb, Weeping Forsythiae Capsule 30 g, respectively; Oriental Waterplantain Rhizome, Red Paeony Root, Bitter Orange 15 g, respectively; Dahurian Patrinia Herb, Sargent gloryvine 20 g, respectively. 1-time/day, add or subtract TCM drugs with the clinical symptoms, 150 mL, 3-time/day, taken orally | 34 | 88.24 | 79.41 | 11.76 | NA | |
| Antibiotics: Ceftriaxone 4.0 g, 1-time/day, Norfloxacin 0.6 g, 1-time/day. Combined with the treatment of liver-protection, diuretics and albumin supplements | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Ceftriaxone 1.0–2.0 g, 1-time/day, Norfloxacin 0.6 g, 1-time/day. Combined with the treatment of liver-protection, albumin supplements and diuretics | 28 | 67.86 | 53.57 | 32.14 | NA | |
| Chen YN (18) [1999]# | ITWM treatment | |||||
| Taking TCM decoction: San Huang Xiao Du Decoction: Spreading Hedyotis Herb 60 g, Baical Skullcap Root, Golden Thread, Rhubarb, Cape Jasmine Fruit 12 g, respectively; Honeysuckle Flower, Mongolian Dandelion Herb, Weeping Forsythiae Capsule 30 g, respectively; Oriental Waterplantain Rhizome, Red Paeony Root, Bitter Orange 15 g, respectively; Dahurian Patrinia Herb, Sargent gloryvine 20 g, respectively. 150 mL, 3-time/day, taken orally | 45 | 93.33 | 86.67 | 6.67 | NA | |
| Antibiotics: Ceftriaxone 1.0–2.0 g, 1-time/day, Norfloxacin 0.6 g 1-time/day. Combined with the treatment of liver-protection, diuretics and albumin supplements | ||||||
| Course of treatment: 7 days | ||||||
| Western medicine treatment | ||||||
| Ceftriaxone 1.0–2.0 g, 1-time/day, Norfloxacin 0.6 g, 1-time/day. Combined with the treatment of liver-protection, diuretics and albumin supplements | 42 | 78.57 | 66.67 | 21.43 | NA | |
| Ren ZJ (19) [2005]# | ITWM treatment | |||||
| Taking TCM decoction: QingWenJieDu Decoction: Baical Skullcap Root 15 g, Honeysuckle Flower 25 g, Mongolian Dandelion Herb 25 g, Cape Jasmine Fruit 15 g, Radix Astragali 30 g, Pilose Asiabell Root 15 g, Largehead Atractylodes Rhizome 15 g, Rhubarb 15 g, Officinal Magnolia Bark 15 g, Danshen Root 20 g, add or subtract TCM drugs with the clinical symptoms, 300 mL, 2-time/day | 42 | 69.05 | 69.05 | 30.95 | NA | |
| Antibiotics: Cefotaxime 2 g, 1-time/8 h. Combined the treatment of liver-protection, symptomatic treatment | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Cefotaxime 2 g, 1-time/8 h. Combined the treatment of liver-protection, symptomatic treatment | 42 | 38.1 | 38.1 | 61.9 | NA | |
| Long SY (20) [2006]+ | ITWM treatment | |||||
| Taking TCM decoction: HuaYuLiShui Decoction: Virgate Wormwood Herb 15 g, Indian Buead 15 g, Agaric 15 g, Largehead Atractylodes Rhizome 15 g, Mongolian Dandelion Herb 15 g, European Verbena 30 g, Spreading Hedyotis Herb 30 g, Giant Knotweed Rhizome 10 g, Zedoary 10 g, Ground Beeltle 10 g, Danshen Root 10 g, Peach Seed 10 g, Bitter Orange 10 g, Pilose Asiabell Root 10 g, Liquoric Root 6 g, add or subtract TCM drugs with the clinical symptoms, 150 mL, 2-time/day | 30 | 90 | 63.33 | 10 | NA | |
| Antibiotics: Ceftriaxone 1 g, 2-time/day. Combined with the treatment of peritoneal lavage | ||||||
| Course of treatment: 60 days | ||||||
| Western medicine treatment | ||||||
| Ceftriaxone 1 g, 2-time/day. Combined with the treatment of peritoneal lavage | 30 | 80 | 50 | 20 | NA | |
| Yang HZ (21) [2006]+ | ITWM treatment | |||||
| Taking TCM decoction: QingXiaXiaoBu Decoction: (I) First step: DaChengQi Decoction: Rhubarb 20–30 g, Mirabilite 9–15 g, Weeping Forsythiae Capsule 30 g, Heartleaf Houttuynia Herb 30 g, Virgate Wormwood Herb 30 g, Cape Jasmine Fruit 24 g, Agaric 24 g, Dahurian Patrinia Herb 30 g. Usage: all herbal boiling into decoction, 1–2 time/day, maintains the times of defecation at 2–3 time/day, add or subtract TCM drugs with the clinical symptoms. Course of treatment: 1 week. (II) Second step: increase the dosage of Turmeric Root-tuber, Red Paeony Root: Rhubarb 6–9 g, Mirabilite 6–12 g, Turtle Shell 15 g, Virgate Wormwood Herb 20 g, Turmeric Root-tuber 30 g, Danshen Root 15 g, Red Paeony Root 30 g, Largehead Atractylodes Rhizome 12 g, Liquoric Root 9 g. Usage: 1-time/day. Combined with ChuanXiongQin injectioin 40–80 mg into glucose injection, 1-time/day, add or subtract TCM drugs with the clinical symptoms. Course of treatment: 1 week | 46 | 91.3 | 76.09 | 8.7 | NA | |
| Antibiotics: Cefoperazone 2 g, 2-time/day | ||||||
| Course of treatment: 2 weeks | ||||||
| Western medicine treatment | ||||||
| Cefoperazone 2 g, 2-time/day. Combined with diuretics, treatment of liver-protection and paracentesis | 46 | 78.3 | 65.22 | 21.7 | NA | |
| Huang YH (22) [2008]* | ITWM treatment | |||||
| Taking TCM decoction: ZhongManFenXiao Wan: Baical Skullcap Root 10 g, Golden Thread 5 g, Common Anemarrhena Rhizome 10 g, Officinal Magnolia Bark 10 g, Bitter Orange 10 g, Pinellia Tuber 10 g, Tangerine Peel 10 g, Indian Buead 15 g, Agaric 15 g, Oriental Waterplantain Rhizome 15 g, Pilose Asiabell Root 15 g, Largehead Atractylodes Rhizome 10 g, Turmeric 10 g, Liquoric Root 5 g, add or subtract TCM drugs with the clinical symptoms, 150 mL, 2-time/day | 40 | 87.5 | 82.5 | 12.5 | NA | |
| Western medicine treatment | ||||||
| Cefotaxime 2 g, 2–3 time/day. Combined with the treatment of liver-protection, diuretics and albumin supplements | 40 | 75 | 65 | 25 | NA | |
| Xie DM (23) [2009]+ | ITWM treatment | |||||
| Taking TCM decoction: JieDuLiShui Decoction: Rhubarb, Golden Thread, Sargent gloryvine, Agaric, Hiraute Shiny Bugleweed Herb, Areca Peel, Areca Seed, 1-time/day | 35 | 77.14 | 51.43 | 22.86 | NA | |
| Antibiotics: a compound that consist of third-generation cephalosporins, broad-spectrum penicillins and β-lactamase inhibitor and Quinolones | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| A compound that consist of third-generation cephalosporins, broad-spectrum penicillins and β-lactamase inhibitor and Quinolones | 28 | 53.57 | 32.14 | 46.43 | NA | |
| Li J (24) [2010]+ | ITWM treatment | |||||
| Taking TCM decoction: Radix Astragali 30 g, Hiraute Shiny Bugleweed Herb 15 g, Plantain Seed 15 g, Areca Peel 30 g, Beautiful Sweetgum Fruit 15 g, Cowherb Seed 30 g, Danshen Root 30 g, Dahurian Patrinia Herb 30 g, Turmeric Root-tuber 10 g, Safflower 10 g, Figwort Root 30 g, Indian Buead 30 g, Common Yam Rhizome 30 g | 40 | 95 | 42.5 | 5 | NA | |
| Antibiotics chosen according to drug sensitivity profile | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Antibiotics chosen according to drug sensitivity profile | 40 | 70 | 25 | 30 | NA | |
| Li WL (25) [2012]# | ITWM treatment | |||||
| Taking TCM decoction: JiaWeiDangGuiShaoYao San: Chinese Angelica 9 g, Red Paeony Root 25 g, Indian Buead12 g, Largehead Atractylodes Rhizome 12 g, Oriental Waterplantain Rhizome 24 g, Coix Seed 30 g, Dahurian Patrinia Herb 15 g, Dwarf Lilyturf Tuber 12 g, Officinal Magnolia Bark 9 g, Areca Peel 15 g, Plantain Seed 30 g, Rice Bean 30 g, 2-time/day | 34 | 94.12 | 70.59 | 5.88 | NA | |
| Antibiotics: Ceftriaxone 3.0 g, 1-time/day. Combined with the treatment of liver-protection, diuretics and symptomatic treatment | ||||||
| Course of treatment: 7 days | ||||||
| Western medicine treatment | ||||||
| Ceftriaxone 3.0 g, 1-time/day. Combined with the treatment of liver-protection, diuretics and symptomatic treatment | 32 | 65.63 | 50 | 34.37 | NA | |
| Qiu L (26) [2012]+ | ITWM treatment | |||||
| Taking TCM decoction: HuoXueYiQi Decoction: Radix Astragali, Indian Buead, Virgate Wormwood Herb 20 g, respectively; Motherwort Herb, Areca Peel, Turtle Shell 15 g, respectively; Tangerine Peel, Red Paeony Root, Oriental Waterplantain Rhizome, Rhubarb, Largehead Atractylodes Rhizome 10 g, respectively. Add or subtract TCM drugs with the clinical symptoms | 40 | 85 | 77.5 | 15 | NA | |
| Antibiotics chosen according to drug sensitivity profile | ||||||
| Course of treatment: 2 weeks | ||||||
| Western medicine treatment | ||||||
| Antibiotics chosen according to drug sensitivity profile and combined with the treatment of liver-protection, diuretics, albumin supplements and maintenance of fluid and electrolyte balance | 40 | 82.5 | 65 | 17.5 | NA | |
| Ren JM (27) [2013]∆ | ITWM treatment | |||||
| Taking TCM decoction: Rhubarb 30 g, 200 mL boiling for 20 min, 100 mL, 2-time/day | 30 | 70 | 70 | 30 | NA | |
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Treatment of liver-protection, diuretics, albumin supplements, blood transfusion, anti-inflammatory and maintenance of fluid and electrolyte balance plus symptomatic treatment | 30 | 70 | 50 | 30 | NA | |
| Liang DJ (28) [2013]+ | ITWM treatment | |||||
| Taking TCM decoction: Self-made TCM Decoction, Rhubarb 10 g, Green Tangerine Peel 10 g, Red Paeony Root 10 g, Ginseng 10 g, Officinal Magnolia Bark 10 g, 200 mL, 2-time/day | 41 | 87.8 | 87.8 | 12.2 | NA | |
| Antibiotics: Ofloxacin 100 mg, taken orally, 3-time/day | ||||||
| Western medicine treatment | ||||||
| Ofloxacin 100 mg, taken orally, 3-time/day | 41 | 68.3 | 68.3 | 31.7 | NA | |
| Lin ZM (29) [2013]+ | ITWM treatment | |||||
| Taking TCM decoction: Self-made Decoction: Ginseng 10 g, Officinal Magnolia Bark 10 g, Rhubarb 10 g, Green Tangerine Peel 10 g, Red Paeony Root 10 g, 200 mL taken orally, 2-time/day | 41 | 95.1 | 87.8 | 4.9 | NA | |
| Antibiotics: Quinolones or third-generation cephalosporins. Combined with treatment of liver-protection, diuretics and maintenance of fluid and electrolyte balance | ||||||
| Course of treatment: 20 days | ||||||
| Western medicine treatment | ||||||
| Quinolones or third-generation cephalosporins. Combined with treatment of liver-protection, diuretics and maintenance of fluid and electrolyte balance | 41 | 80.5 | 68.29 | 19.5 | NA | |
| Chen G (30) [2015]+ | ITWM treatment | |||||
| Taking TCM decoction: WenYangJieDu Decoction: Medicinal Indianmulberry Root 30 g, Epimedium Herb 15 g, Radix Astragali 20 g, Danshen Root 15 g, Rhubarb 5 g, Indian Buead 15 g, Baical Skullcap Root 10 g, Dahurian Patrinia Herb 10 g, Liquoric Root 5 g, 100 mL, 3-time/day | 19 | 94.73 | 68.42 | 5.27 | NA | |
| Antibiotics: Cefoperazone 2 g, 2-time/day | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| According the results of drug sensitivity choose antibiotics, or Cefoperazone 2 g, 2-time/day and diuretics after paracentesis | 17 | 70.59 | 23.53 | 29.41 | NA | |
| Wan ZM (31) [2015]# | ITWM treatment | |||||
| Taking TCM decoction: FuFangChaiShaoChengQi Decoction: Chinese Thorowax Root 12 g, Baical Skullcap Root 10 g, Green Tangerine Peel 12 g, Officinal Magnolia Bark 10 g, Rhubarb 10 g, Sargent gloryvine 30 g, Dahurian Patrinia Herb 30 g | 60 | 58.33 | 58.33 | 41.67 | 18.33 | |
| Antibiotics: Cefotaxime 2.0 g, 3-time/day | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Cefotaxime 2.0 g, 3-time/day, combined with treatment of liver-protection, symptomatic treatment and intestinal flora balance rebuilding | 60 | 40 | 40 | 60 | 35 | |
| Gao J (44) [1996]+ | ITWM treatment | |||||
| TCM enema: Rhubarb 12 g, Baical Skullcap Root 15 g, Golden Thread 10 g, Danshen Root 30 g, Red Paeony Root 30 g, 100 mL, TCM enema, 1-time/night | 24 | 66.7 | 66.7 | 33.3 | NA | |
| Antibiotics: Ampicillin 3.0 g, 2-time/day, or Ceftazidime 1.0 g, 2-time/day, associated with the treatment of liver-protection and symptomatic treatment | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Ampicillin 3.0 g, 2-time/day, or Ceftazidime 1.0 g, 2-time/day, associated with the treatment of liver-protection and symptomatic treatment | 18 | 33.3 | 33.3 | 66.7 | NA | |
| Liu LQ (45) [1998]+ | ITWM treatment | |||||
| TCM enema: Honeysuckle Flower, Mongolian Dandelion Herb, Indigowoad Leaf, Heartleaf Houttuynia Herb, Chinese Angelica, Danshen Root, Frankincense, Myrrh 15 g, respectively. 200 mL, retention enemas for 2 h, 1-time/day | 36 | 75 | 61.11 | 25 | 25 | |
| Antibiotics: Amikacin, Ampicillin, Ampicillin, third-generation cephalosporins | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Amikacin, Ampicillin, third-generation cephalosporins, associated with paracentesis and symptomatic treatment | 36 | 47.2 | 38.89 | 52.78 | 52.78 | |
| Tu YY (46) [2006]+ | ITWM treatment | |||||
| TCM enema: Rhubarb, Honeysuckle Flower, Mongolian Dandelion Herb 30 g, respectively. 100 mL, retention enemas for 0.5 h, 1-time/day | 23 | 82.6 | 34.78 | 17.4 | 8.7 | |
| Antibiotics: Cefotaxime 2.0 g, 2-time/day associated with the treatment of liver-protection, symptomatic treatment, diuretics | ||||||
| Course of treatment: 2 weeks | ||||||
| Western medicine treatment | ||||||
| Cefotaxime 2.0 g, 2-time/day. Combined with the treatment of liver-protection, symptomatic treatment and diuretics | 25 | 36 | 20 | 64 | 32 | |
| Wu L (56) [2006]+ | ITWM treatment | |||||
| Peritoneal lavage using IMS100A-Colonic irrigation machine. The peritoneal lavage consisted of a douche including: sodium chloride 50.4g, calcium chloride 3.2g, magnesium chloride 1.6g, lactate 50g, glucose 250g, combined with 1000ml distilled water. After the peritoneal lavage, a preparation enema included Rhubarb, Red Paeony Root, Virgate Wormwood Herb, Cape Jasmine Fruit, Giant Knotweed Rhizome | 64 | 85.9 | 85.9 | 14.1 | NA | |
| Course of treatment: 12 weeks | ||||||
| Western medicine treatment | ||||||
| Treatment of liver-protection, cholagogue, diuretics, hemostasis and anti-inflammatory. | 50 | 64 | 64 | 36 | NA | |
| Han J (52) [2007]+ | ITWM treatment | |||||
| TCM compression on umbilicus: QiReHuaYu San: Red Paeony Root 30 g, Honeysuckle Flower 30 g, Dahurian Patrinia Herb 30 g, Yanhusuo 15 g, Lightyellow Sophora Root 30 g, Rhubarb 12 g, Spreading Hedyotis Herb 30 g, Peach Seed 20 g. Mixing batter use honey, compression on umbilicus for 8 h | 30 | 90 | 60 | 10 | NA | |
| Antibiotics: Cefoperazone 2.0 g, 2-time/day | ||||||
| Course of treatment: 20 days | ||||||
| Western medicine treatment | ||||||
| Cefoperazone 2.0 g, 2-time/day | 30 | 76.6 | 43.33 | 23.4 | NA | |
| Tian X (53) [2008]+ | ITWM treatment | |||||
| TCM compression on umbilicus: Rhubarb 10 g, Oriental Waterplantain Rhizome 20 g, Plantain Seed 20 g, add or subtract TCM drugs with the clinical symptoms | 39 | 84.62 | 64.1 | 15.38 | 5.13 | |
| Antibiotics: Cefoperazone 2.0 g, Mezlocillin 2.5 g, 2-time/day | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Cefoperazone 2.0 g, Mezlocillin 2.5 g, 2-time/day | 39 | 71.79 | 53.85 | 28.21 | 7.69 | |
| Xing YM (47) [2009]+ | ITWM treatment | |||||
| TCM enema: Golden Thread 9 g, Baical Skullcap Root 6 g, Cape Jasmine Fruit 9 g, Mongolian Dandelion Herb 30 g, Barbed Skullcap Herb 15 g, Spreading Hedyotis Herb 30 g, Red Paeony Root 12 g, Danshen Root 20 g, Rhubarb 9 g, add or subtract TCM drugs with the clinical symptoms.100–150 mL, retention enemas half an hour, 2-time/day | 38 | 84.2 | 52.63 | 15.8 | NA | |
| Course of treatment: 2 weeks | ||||||
| Western medicine treatment | ||||||
| According the results of drug sensitivity choose antibiotics, or Cefotaxime 2 g. Combined with treatment of liver-protection, blood transfusion, albumin supplements and diuretics | 30 | 63.3 | 40 | 36.7 | NA | |
| Ji XL (48) [2009]+ | ITWM treatment | |||||
| TCM enema: Rhubarb 20 g, Indigowoad Root 30 g, Lightyellow Sophora Root 20 g, Red Paeony Root 20 g, Halloysit 15 g. Combined with Lactulose 30 g, Bacillus Licheniformis 0.6 g, 100 mL, TCM enema, 1-time/day. Combined with Western medicine treatment: treatment of liver-protection, diuretics, paracentesis, immune-modulatory and microbiological agents |
31 | 70.9 | 25.81 | 29.1 | NA | |
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Combined with treatment of liver-protection, diuretics, paracentesis, and immune-modulatory, microbiological agents | 31 | 32.2 | 12.9 | 67.8 | NA | |
| Liu HL (49) [2009]+ | ITWM treatment | |||||
| TCM enema: Honeysuckle Flower 30 g, Rhubarb 20 g, Mongolian Dandelion Herb 60 g, Giant Knotweed Rhizome 20 g, Oyster Shell 30 g, Spreading Hedyotis Herb 50 g, Danshen Root 30 g, Parslane Herb 30 g, Dahurian Patrinia Herb 20 g, Golden Thread 10 g, 200–300 mL, retention enemas for 4 h |
40 | 90 | 65 | 10 | NA | |
| Antibiotics: Ceftazidime 3.0 g, 2-time/day. Combined with the treatment of liver-protection, diuretics and symptomatic treatment | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Ceftazidime 3.0 g, 2-time/day. Combined with the treatment of liver-protection, diuretics and symptomatic treatment | 40 | 75 | 45 | 25 | NA | |
| Jing XH (50) [2010]+ | ITWM treatment | |||||
| TCM enema: Rhubarb 10 g, Baical Skullcap Root 10 g, Dahurian Patrinia Herb 30 g, Mongolian Dandelion Herb 30 g, 1-time/day. Combined with XueBiJing injection 60 mL, 1-time/day | 32 | 90.6 | 68.75 | 9.4 | NA | |
| Antibiotics: Ceftazidime 2 g, 1-time/day | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Ceftazidime 2 g, 1-time/day | 28 | 78.6 | 46.43 | 21.4 | NA | |
| Ma YP (51) [2013]+ | ITWM treatment | |||||
| TCM enema: JieDuGuanChangYe: Rhubarb 30 g, Honeysuckle Flower, Chinese Pulsatilla Root, Mongolian Dandelion Herb, Danshen Root, Red Paeony Root 20 g, respectively; Green Tangerine Peel, Officinal Magnolia Bark 10 g, respectively. 200 mL, 2-time/day, 30 minutes each time | 50 | 90 | 56 | 10 | NA | |
| Antibiotics: Ceftriaxone or Cefoperazone, 2-time/day. Combined with anti-inflammatory, treatment of liver-protection, blood transfusion, albumin supplements | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Ceftriaxone or Cefoperazone, 2-time/day. Combined with anti-inflammatory, treatment of liver-protection, blood transfusion, albumin supplements | 50 | 76 | 36 | 24 | NA | |
| Li GH (54) [2014]# | ITWM treatment | |||||
| TCM compression on umbilicus: SiHuangMiShuiGao: Golden Thread, Baical Skullcap Root, Rhubarb, Borneol, Frankincense, Dragon’s Blood, Myrrh 10 g, respectively; Lightyellow Sophora Root 20 g, Common Clubmoss Herb 15 g, Garden Balsam Stem 20 g, mixing batter use honey, compressing on umbilicus | 35 | 91.43 | 88.57 | 8.57 | NA | |
| Antibiotics: Quinolones or third-generation cephalosporins. Combined with diuretics, treatment of liver-protection, maintain fluid and electrolyte balance | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Quinolones or third-generation cephalosporins. Combined with diuretics, treatment of liver-protection and maintenance of fluid and electrolyte balance | 35 | 71.43 | 62.86 | 28.57 | NA | |
| Yang M (55) [2015]+ | ITWM treatment | |||||
| TCM compression on umbilicus: QiReHuaYu San: Dahurian Patrinia Herb 30 g, Peach Seed 20 g, Rhubarb 12 g, Honeysuckle Flower 30 g, Lightyellow Sophora Root 30 g, Spreading Hedyotis Herb 30 g, Yanhusuo 15 g, Red Paeony Root 30 g. Mixing batter use honey | 65 | 92.3 | 40 | 7.7 | NA | |
| Antibiotics: Cefoperazone 2.0g, 2-time/day | ||||||
| Course of treatment: 1 month | ||||||
| Western medicine treatment | ||||||
| Antibiotics: Cefoperazone 2.0 g, 2-time/day | 48 | 73.8 | 43.75 | 26.2 | NA | |
| Peng YP (57) [2015]∆ | ITWM treatment | |||||
| TCM enema: Heartleaf Houttuynia Herb 30 g, 100 mL TCM enema 1-time/day | 30 | 63 | 40 | 37 | NA | |
| Antibiotics: Cefuroxime 1.5 g, 1-time/day | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Levofloxacin 0.4 g, and Cefuroxime 1.5 g, 1-time/day | 28 | 46 | 32.14 | 54 | NA | |
| Ji JJ (32) [1999]* | ITWM treatment | |||||
| Chinese patent medicine: ShuangHuangLian injection 3.6–4.8 g into 5% Glucose injection 250 mL. | 42 | 93 | 83.33 | 7 | NA | |
| Antibiotics: Piperacillin 4 g, 2-time/day. Ofloxacin 0.2 g, 2-time/day. Combined with the treatment of liver-protection, diuretics and albumin supplements | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Piperacillin 4 g, 2-time/day. Ofloxacin 0.2 g, 2-time/day. Combined with the treatment of liver-protection, diuretics and albumin supplements | 40 | 78 | 60 | 22 | NA | |
| Zhang YH (33) [2002]* | ITWM treatment | |||||
| Chinese patent medicine: ShuangHuangLian injection 3.6–4.8 g into 5% glucose injection 250 mL | 22 | 96 | 81.82 | 4 | NA | |
| Antibiotics: Piperacillin 4 g, 2-time/day. Ofloxacin 0.2 g, 2-time/day. Combined with the treatment of liver-protection, diuretics and albumin supplements | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Piperacillin 4 g, 2-time/day. Ofloxacin 0.2 g, 2-time/day. Combined with the treatment of liver-protection, diuretics and albumin supplements | 20 | 80 | 60 | 20 | NA | |
| Song XX (34) [2008]* | ITWM treatment | |||||
| Chinese patent medicine: QingKaiLing injection, 1,000 mg 1-time/day | 46 | 56.52 | 56.52 | 43.48 | NA | |
| Antibiotics: Cefoperazone or Cefotaxime 2.0 g, 2-time/day. Combined with the treatment of liver-protection, diuretics and symptomatic treatment | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Antibiotics: Cefoperazone or Cefotaxime 2.0 g, 2-time/day. Combined with the treatment of liver-protection, diuretics and symptomatic treatment | 41 | 36.59 | 36.59 | 63.41 | NA | |
| Tan ZB (35) [2008]* | ITWM treatment | |||||
| Chinese patent medicine: TanReQing injection: 20 mL into 5% 250 mL Glucose injection, 1-time/day | 40 | 95 | 95 | 5 | NA | |
| Antibiotics: Cefotaxime 2 g, 1-time/8 h | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Cefotaxime 2 g, 1-time/8 h. Combined with the treatment of liver-protection, diuretics and albumin supplements | 30 | 76.67 | 76.67 | 23.33 | NA | |
| Zhang YQ (36) [2010]* | ITWM treatment | |||||
| Chinese patent medicine: XueBiJing injection: 50 mL into 100 mL normal saline, 1-time/12 h | 90 | 92.22 | 8.89 | 7.78 | NA | |
| Antibiotics: Ceftriaxone 2 g, 1-time/day | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Ceftriaxone 2 g, 1-time/day. Combined with the treatment of liver-protection, diuretics and correction of ionic disorders | 78 | 80.77 | 2.56 | 19.23 | NA | |
| Wang J (37) [2010]* | ITWM treatment | |||||
| Chinese patent medicine: XueBiJing injection: 50 mL into 100 mL normal saline, 2-time/day | 30 | 93.3 | 66.67 | 6.7 | NA | |
| Antibiotics: Ceftriaxone 2 g, 1-time/day | ||||||
| Course of treatment: 7 days | ||||||
| Western medicine treatment | ||||||
| Ceftriaxone 2 g, 1-time/day | 30 | 70 | 46.67 | 30 | NA | |
| Shu Q (38) [2011]* | ITWM treatment | |||||
| Chinese patent medicine: XueBiJing injection: 50 mL into 100 mL normal saline, 1-time/day | 32 | 87.5 | 31.25 | 12.5 | NA | |
| Antibiotics: the third-generation cephalosporins | ||||||
| Course of treatment: 14 days | ||||||
| Western medicine treatment | ||||||
| Third-generation cephalosporins. Combined with the treatment of liver-protection and symptomatic treatment | 34 | 70.6 | 23.53 | 29.4 | NA | |
| Zheng J (39) [2012]* | ITWM treatment | |||||
| Chinese patent medicine: XueBiJing injection: 50 mL into 100 mL normal saline, 1-time/12 h | 31 | 90.32 | 77.42 | 9.68 | NA | |
| Antibiotics: mainly depend on Levofloxacin and the third-generation cephalosporins | ||||||
| Course of treatment: 14 days | ||||||
| Western medicine treatment | ||||||
| Mainly depend on Levofloxacin and the third-generation cephalosporins. Combined with the treatment of liver-protection, diuretics and albumin supplements | 32 | 93.75 | 40.62 | 6.25 | NA | |
| Zhang RW (40) [2014]* | ITWM treatment | |||||
| Chinese patent medicine: Xuebijing injection: 50 mL into 100 mL normal saline, 2-time/day | 32 | 87.5 | 62.5 | 12.5 | NA | |
| Antibiotics: Ceftazidime 2 g, 1-time/day | ||||||
| Course of treatment: 28 days | ||||||
| Western medicine treatment | ||||||
| Ceftazidime 2 g, 1-time/day. Combined with conventional treatment including liver-protection and diuretics | 32 | 68.75 | 31.25 | 31.25 | NA | |
| Wang YL (41) [2015]* | ITWM treatment | |||||
| Chinese patent medicine: XueBiJing injection: 50 mL into 100 mL normal saline, 1-time/day. | 44 | 90.91 | 61.36 | 9.09 | NA | |
| Antibiotics: Imipenem cilastatin 0.5 g, 3-time/day; paracentesis ≤2,000 mL/day. Combined with Imipenem cilastatin 0.5 g inject into abdomen | ||||||
| Course of treatment: 7 days | ||||||
| Western medicine treatment | ||||||
| Imipenem cilastatin 0.5 g, 3-time/day; paracentesis ≤2,000 mL/day. Combined with Imipenem cilastatin 0.5 g inject into abdomen | 44 | 75 | 34.09 | 25 | NA | |
| Ma L (42) [1999]* | ITWM treatment | |||||
| Chinese patent medicine: ChuanHuNing injection peritoneal lavage: 3,000 mL, inject ChuanHuNing injection into abdomen, 40 mL + 2% Metronidazole 1,000 mL | 57 | 91.23 | 84.21 | 8.77 | NA | |
| Antibiotics: Ceftriaxone 4.0 g peritoneal lavage | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Metronidazole lavage and Metronidazole, Ceftriaxone inject into abdomen. Combined with conventional liver-protection, diuretics and correct electrolyte turbulence | 51 | 62.75 | 43.14 | 37.25 | NA | |
| Zhang NN (43) [2015]* | ITWM treatment | |||||
| Chinese patent medicine: ShenLingBaiZhu granule: White Hyacinth Bean, Largehead Atractylodes Rhizome, Indian Buead, Liquoric Root, Platycodon Root, Semen Nelumbinis, Ginseng, Common Yam Rhizome, Coix Seed, 3-time/day | 33 | 72.73 | 63.64 | 27.27 | NA | |
| Antibiotics: Cefoperazone 3 g, 2-time/day. Combined with conventional liver-protection, diuretics and treatment to improve circulation | ||||||
| The time of the treatment depended on the patient's condition | ||||||
| Western medicine treatment | ||||||
| Cefoperazone 3 g, 2-time/day. Combined with conventional liver-protection, diuretics and treatment to improve circulation | 32 | 46.88 | 37.5 | 53.12 | NA |
∆, study that used single-TCM drug; *, study that used TCM compound that have been proven by the China Food and Drug Administration; #, study that used the classical TCM compound; +, study that used the self-made TCM compound. ITWM, integration of traditional and Western medicine; TCM, traditional Chinese medicine; NA, not available.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.08.10). Dr. Qi serves as an Editor-in-Chief of AME Medical Journal. Andrea Mancuso serves as an unpaid editorial board member of AME Medical Journal from Mar 2017 to Mar 2019. Fernando Gomes Romeiro serves as an unpaid editorial board member of AME Medical Journal from Apr 2017 to Apr 2019. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ge PS, Runyon BA. Treatment of Patients with Cirrhosis. N Engl J Med 2016;375:767-77. [Crossref] [PubMed]
- Gines P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology 1987;7:122-8. [Crossref] [PubMed]
- Rimola A, Garcia-Tsao G, Navasa M, et al. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. International Ascites Club. J Hepatol 2000;32:142-53. [Crossref] [PubMed]
- Wiest R, Krag A, Gerbes A. Spontaneous bacterial peritonitis: recent guidelines and beyond. Gut 2012;61:297-310. [Crossref] [PubMed]
- Bichet D, Szatalowicz V, Chaimovitz C, et al. Role of vasopressin in abnormal water excretion in cirrhotic patients. Ann Intern Med 1982;96:413-7. [Crossref] [PubMed]
- European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol 2010;53:397-417. [Crossref] [PubMed]
- Angeloni S, Leboffe C, Parente A, et al. Efficacy of current guidelines for the treatment of spontaneous bacterial peritonitis in the clinical practice. World J Gastroenterol 2008;14:2757-62. [Crossref] [PubMed]
- Runyon BA, Committee AP. Management of adult patients with ascites due to cirrhosis: an update. Hepatology 2009;49:2087-107. [Crossref] [PubMed]
- Pericleous M, Sarnowski A, Moore A, et al. The clinical management of abdominal ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: a review of current guidelines and recommendations. Eur J Gastroenterol Hepatol 2016;28:e10-8. [Crossref] [PubMed]
- Lv CL, Hang GQ, Xu Y. Clinical distribution and drug resistance analysis of pathogens causing liver cirrhosis complicated with spontaneous bacterial peritonitis. International Journal of Laboratory Medicine 2012;(10):1215-6.
- Zheng L, Yang YD, Kong HS, et al. The bacterial and drug resistance in cirrhotic patients complicated with spontaneous bacterial peritonitis. Chinese Journal of Infectious Diseases 2001;19:181.
- Zhou DH, Lin LZ, Zhou YQ. Analysis of short-term therapeutic efficacy of integrated traditional and Western medicine in treating non-small cell lung cancer. Zhongguo Zhong Xi Yi Jie He Za Zhi 2005;25:1061-5. [PubMed]
- Heng M, Tu J, Hao Y, et al. Effects of Integrated Traditional Chinese and Western Medicine for the Treatment of Lupus Nephritis: A Meta-Analysis of Randomized Trials. Evid Based Complement Alternat Med 2016;2016:1502107.
- Chen L, Lu ZP. Randomized controlled trial of integrated traditional Chinese and western medicine treatment for posthepatitic cirrhotic ascites: a systematic review. Zhonghua Gan Zang Bing Za Zhi 2011;19:205-9. [PubMed]
- Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12. [Crossref] [PubMed]
- Li QF, Wang HS, Shen JX, et al. The efficiency of Dachengqi Tang in associated with norfloxacin in the treatment of spontaneous bacterial peritonitis. Chin J Inte Trad West Med Liver Dis 1995;5:32.
- Chen YN, Jiang GH, Jin BS. Integration of traditional and Western medicine in the treatment of spontaneous bacterial peritonitis in 34 patients. Chinese Journal of Integrated Traditional and Western Medicine 1997;17:55.
- Chen YN, Jiang GH, Jin BS, et al. Sanhuangxiaoduyin in associated with Western medicine in the treatment of spontaneous bacterial peritonitis in 45. Chinese Journal of Integrated Traditional and Western Medicine in Intensive and Critical 1999;6:270-1.
- Ren ZJ, Liu M, Tang SB, et al. Evaluation of the combination treatment of traditional Chinese medicine and western medicine on spontaneous bacterial peritonitis associated with hepatocirrhosis. Chinese Journal of Infection Control 2005;4:30-2.
- Long SY, He HH. The treatment efficiency of traditional medicine integrated with Western medicine in the treatment of spontaneous bacterial peritonitis. Journal of Emergency in Traditional Chinese Medicin 2006;15:481-2.
- Yang HZ, Xie HP, Wang YZ, et al. Qingxiaxiaobusifaerbu in associate with antibiotic in the treatment of spontaneous bacterial peritonitis. China Journal of Experimental Traditional Medical Formulae 2006;12:57-9.
- Huang YH, Xiong Y, Yang H, et al. Zhongmanfenxiaowan in associate with cefotaxime sodium in the treatment spontaneous bacterial peritonitis in 40 cirrhotic patients. Chinese Journal of Information on Traditional Chinese Medicine 2008;15:70-1.
- Xie DM, Cheng ZW, Pan JZ, et al. Treatment of 35 cases of liver cirrhosis complicated with spontaneous bacterial peritonitis. Jiangxi Journal of Traditional Chinese Medicine 2009;40:24-5.
- Li J. Combination of traditional Chinese and Western medicine in the treatment of 40 cases of liver cirrhosis complicated with spontaneous bacterial peritonitis. Chinese Journal of Traditional Medical Science and Technology 2010;17:547-8.
- Li WL, Wang CD, Hong XB, et al. Curative effect observation of Jiaweidangguishaoyaosan in the treatment of spontaneous bacterial peritonitis. Journal of Emergency in Traditional Chinese Medicine 2012;21:1155-6.
- Qiu L, Chen JL. Combination of traditional Chinese medicine and Western medicine in the treatment of liver cirrhosis complicated with spontaneous bacterial peritonitis. Lishizhen Medicine and Materia Medica Research 2012;23:2921-2.
- Ren JM, Wu ZL. Rhubarb in the treatment and nursing of liver cirrhosis complicated with spontaneous bacterial peritonitis. Research and Practice of Chinese Medicines 2013;27:88.
- Liang DJ, Zhao XL. The effects of combination of Chinese and western medicine treatment for spontaneous bacterial peritonitis. China medicine and pharmacy 2013;3:186-7.
- Lin ZM, Wang BB, Lin XF. Methods to observe the traditional Chinese and Western treatment of liver cirrhosis spontaneous peritonitis effect. Chinese Journal of Rural Medicine and Pharmacy 2013;20:51-2.
- Chen G, Luo JX, Zhou JL, et al. Effect of Wenyang Jiedu Recipe Combined with Peritoneal Lavage Therapy on IL-10,IL-18 Levels of Cirrhosis Incorporated Spontaneous Bacterial Peritonitis Patients. Journal of Sichuan of Traditional Medicine 2015;33:73-6.
- Wan ZM, Zheng X, Zhu L. Clinical observation on the treatment of 60 cases of wanxue and spontaneous bacterial peritonitis with Chinese and Western Medicine. Medical Information 2015;28:30.
- Ji JJ, Dai MQ. Shuanghuanglian Injection in adjuvant treatment of hepatic cirrhosis complicated with spontaneous bacterial peritonitis. Chinese Journal of New Drug and Clinical Remedies 1999;18:399-400.
- Zhang YH, Qi Y, Lin CL. Shuanghuanglian Injection in adjuvant treatment of hepatic cirrhosis complicated with spontaneous bacterial peritonitis. Information on Traditional Chinese Medicine 2002;19:30.
- Song XX. Qingkailing combined with treatment of spontaneous bacterial peritonitis in 46 cases. Jiangxi Journal of Traditional Chinese Medicine 2008;48.
- Tan ZB. The experience of Tanreqing combined with cefotaxime sodium in the treatment of liver cirrhosis complicated with spontaneous peritonitis. Journal of Emergency in Traditional Chinese Medicine 2008;17:1613-4.
- Zhang YQ, Fu JF. Clinical evaluation of Xuebijing in treatment of liver cirrhosis complicated with spontaneous bacterial peritonitis. Progress in Modern Biomedicine 2010;10:2792-4.
- Wang J, Li F. Clinical evaluation of Xuebijing in treatment of liver cirrhosis complicated with spontaneous bacterial peritonitis. Capital Medicine 2010;(4):49-50.
- Shu Q, Liu J, Peng L, et al. 32 cases of Xuebijing injection in the treatment of liver cirrhosis with spontaneous bacterial peritonitis. Chinese Journal of Integrated Traditional and Western Medicine on Digestion 2011;19:120-2.
- Zheng J, He P. Study on the effect of Xuebijing injection in the treatment of spontaneous bacterial peritonitis. Chinese Community Doctors 2012;14:213-4.
- Zhang RW, Leng AM. Clinical effect of Xuebijing injection on spontaneous bacterial peritonitis. Medical Journal of West China 2014;26:1656-8.
- Wang YL, Zheng YQ, Xin LV, et al. Clinical study on Xuebijing Injection combined with imipenem in treatment of liver cirrhosis complicated with spontaneous bacterial peritonitis. Drugs & Clinic 2015;30:1482-6.
- Ma L, Zhang SY, Zhao WX, et al. Treatment of 57 cases of liver cirrhosis complicated with spontaneous bacterial peritonitis by peritoneal lavage and injection of Western and Chinese Medicine. Chinese Journal of Integrated Traditional and Western Medicine 1999;19:746.
- Zhang NN, Xu L, Liu P. Shenlingbaizhu granules in the treatment of spontaneous bacterial peritonitis. Journal of Emergency in Traditional Chinese Medicine 2015;24:2252-4.
- Gao J. Efficacy of traditional Chinese medicine enema in treatment of liver cirrhosis complicated with ascites and primary peritonitis. Chinese Journal of Integrated Traditional and Western Medicine in Intensive and Critical 1996;3:399-400.
- Liu LQ, Zhong Y. The treatment efficiency of traditional medicine integrated with Western medicine in the treatment of spontaneous bacterial peritonitis. Hubei Journal of Traditional Chinese Medicine 1998;20:25.
- Tu YY, Xu J, Yuan F, et al. The effectiveness of traditional Chinese medicine enema-threpy in the treatment of spontaneous bacterial peritonitis. Guangxi Journal of Traditional Chinese Medicine 2006;29:43-4.
- Xing YM. Clinical observation on the treatment of liver cirrhosis complicated with spontaneous bacterial peritonitis. World Health Digest 2009;6:208-9.
- Ji XL, Ji RY. Clinical study of traditional Chinese medicine and Western medicine in the treatment of liver cirrhosis complicated with ascites and spontaneous bacterial peritonitis. Chinese Journal of New Clinical Medicine 2009;2:276-8.
- Liu H. Traditional Chinese Medicine Enema with antibiotics in the treatment of 40 cases of liver cirrhosis spontaneous bacterial peritonitis. Modern Traditional Chinese Medicine 2009;29:12-4.
- Jing XH. The efficiency of Xuebijing in associated with traditional Chinese medicine enema-therapy in the treatment of spontaneous bacterial peritonitis. Liaoning Journal of Traditional Chinese Medicine 2010;37:1079-80.
- Ma YP, Peng J. The treatment of enema association with antibiotic in cirrhotic patients with spontaneous bacterial peritonitis in 50 cases. Chinese Journal of Integrated Traditional and Western Medicine on Liver Diseases 2013;23:363-4.
- Han J, Wang LR. Efficacy of Chinese medicine combined with antibiotics in the treatment of liver cirrhosis complicated with ascites complicated with spontaneous bacterial peritonitis. Liaoning Journal of Traditional Chinese Medicine 2007;34:1594-5.
- Tian X, Wu XF. Efficacy of antibiotics combined with traditional Chinese medicine on the treatment of spontaneous bacterial peritonitis. Chinese Journal of Clinical Infectious Diseases 2008;1:106-7.
- Li GH, Zhang JC, Li JJ, et al. Sihuangmishuigao combined with western medicine for the treatment of liver cirrhosis complicated with spontaneous bacterial peritonitis randomized controlled study. Journal of Practical Traditional Chinese Internal Medicine 2014;28:118-20.
- Yang M. Effective observation on treating ascites due to cirrhosis plus spontaneous bacterial peritonitis with TCM plus antibiotics. Clinical Journal of Chinese Medicine 2015;7:104-5.
- Liang WU, Wang Y, Zhang ZG, et al. Clinical use of colon-therapy-system combined with Chinese medicines in fulminant hepatitis associated with spontaneous bacterial peritonitis. Chin J Rehabilitation 2006;21:326-8.
- Peng YP. The efficiency of Yuxingcao enema-therapy in the treatment of spontaneous bacterial peritonitis. Medical Equipment 2015;28:36-7.
- Garvey M. Chinese Medicine History and Contemporary Practice in the West. Journal of Health Science 2014;2:284-90.
- Jiang WY. Therapeutic wisdom in traditional Chinese medicine: A perspective from modern science. Discov Med 2005;5:455-61. [PubMed]
- Cui YL, Wang L, Tian ZT, et al. Effect of rhubarb pre-treatment on intestinal microcirculation in septic rats. Am J Chin Med 2014;42:1215-27. [Crossref] [PubMed]
- Wang L, Yang CL, Or TC, et al. Differential effects of Radix Paeoniae Rubra (Chishao) on cytokine and chemokine expression inducible by mycobacteria. Chin Med 2011;6:14. [Crossref] [PubMed]
- Zhang W, Dai SM. Mechanisms involved in the therapeutic effects of Paeonia lactiflora Pallas in rheumatoid arthritis. Int Immunopharmacol 2012;14:27-31. [Crossref] [PubMed]
- Liu MW, Wang YH, Qian CY, et al. Xuebijing exerts protective effects on lung permeability leakage and lung injury by upregulating Toll-interacting protein expression in rats with sepsis. Int J Mol Med 2014;34:1492-504. [Crossref] [PubMed]
- Ma K. Research progress of drug-induced liver injury induced by traditional Chinese Medicine. Guangming Journal of Chinese Medicine 2015;(4):907-11.
- Hu WX. Traditional Chinese medicine induced renal injury. Bulletin of Medical Postgraduate 2000;13:268-70.
- Teschke R, Wolff A, Frenzel C, et al. Herbal traditional Chinese medicine and its evidence base in gastrointestinal disorders. World J Gastroenterol 2015;21:4466-90. [PubMed]
- Wang G, Mao B, Xiong ZY, et al. The quality of reporting of randomized controlled trials of traditional Chinese medicine: a survey of 13 randomly selected journals from mainland China. Clin Ther 2007;29:1456-67. [Crossref] [PubMed]
- Zhang L, Yan J, Liu X, et al. Pharmacovigilance practice and risk control of Traditional Chinese Medicine drugs in China: current status and future perspective. J Ethnopharmacol 2012;140:519-25. [Crossref] [PubMed]
Cite this article as: Wang R, Han D, Sun M, Teschke R, Yang SS, Mendez-Sanchez N, Yang Z, Li M, Mancuso A, Romeiro FG, Guo X, Qi X; written on behalf of the AME Liver Disease Collaborative Group. Efficacy and safety of integration of traditional and Western medicine for the treatment of spontaneous bacterial peritonitis in liver cirrhosis: a systematic review. AME Med J 2017;2:138.