
The technique of S2-alar-iliac screw fixation: a literature review
Introduction
Distal fixation of the end of thoracolumbar deformities can be challenging. Isolated S1-pedicle screw fixation is reported to have a high rate of pullout failure or breakage (up to 44%), and pseudarthrosis (up to 33%) (1-3). Some modified techniques have been introduced to improve the fixation strength and decrease the failure rate, including traditional iliac fixation, S1 cemented augmentation, S1 bicortical screws and S2 alar screw fixation (4-6). Traditional iliac screw fixation has improved resistance to pullout (7). The combination of the iliac screws and S1-pedicle screws for distal fixation can protect the S1 screw from failure and increase the rate of fusion (8,9).
The traditional iliac screw entry point is at the posterior superior iliac spine and requires considerable soft tissue dissection in order to remove the bone block for screw insertion. Iliac screws sit in a lateral position compared to the S1 pedicle screw; thus, an offset connector is used to connect the iliac screw to the rod. However, this has the potential to increase the risk of wound complications, and increase post-operative pain in patient secondary to the extensive soft tissue manipulation. Moreover, the short distance between the screw end and skin may result in instrumentation prominence and subsequent pain (9,10).
To overcome these challenges, a novel S2-alar-iliac (S2AI) screw fixation technique has been developed (11,12). The S2AI screw entry point is medial to the iliac screw, requiring less soft tissue dissection, and avoiding instrumentation prominence. As such, this technique is a potential alternative fixation to Galveston or iliac screw fixation.
Anatomy
In order to illustrate the feasibility of the S2AI screw fixation and provide instructive data, several anatomic studies were conducted on computed tomography (CT) and cadaveric specimens (11,13-16). Parameters measured included (Figure 1): SL/STL: screw length or screw trajectory length; SLIS: screw length of the intrasacral part; IW: iliac width as defined by the narrowest iliac width measured between the inner cortices in the transverse plane; α: angle between screw trajectory and horizontal line in the sagittal plane; β: lateral trajectory angulation in the transverse plane; and γ: angle between screw trajectory and middle vertical line in the coronal plane. Typical S2AI screw trajectory parameters published previously (11-14,17) are summarized in Table 1. The angle between screw trajectory and horizontal line in the sagittal plane ranges from 27.5° to 48.8°, and averages 27.5° to 39.0°. The lateral trajectory angulation in the transverse plane ranges from 30.8° to 67.3°, and averages 32.4° to 52.2°. The angle between screw trajectory and middle vertical line in the coronal plane ranges from 19° to 49.2°, and averages 29.0° to 34.6°.
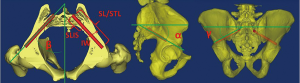
Table 1
| Parameters | O’Brien 2009 | O’Brien 2010 | Chang 2009 | Zhu 2013 | Zhu 2013 | Yamada 2017 | Yamada 2017 |
|---|---|---|---|---|---|---|---|
| Countries | USA | USA | USA | China | China | Japan | Japan |
| Method of evaluation | Fresh cadaveric spine (n=10) | Fresh cadaveric spine (n=8) | CT (n=20) | CT (male) (n=30) | CT (female) (n=30) | CT (male) (n=40) | CT (female) (n=40) |
| SL/STL (mm) | |||||||
| Left | 84.0±10.7 [70–100] | 89.5±18.7 (69–118.2) | 106.3±8.9# (88.3–124) | 121.3±8.3# | 114.8±9.4# | 121.5±10.3 | 113.8±9.6 |
| Right | 84.0±10.7 [70–100] | 95.4±20.4 (71.3–120) | 103.7±9.9# (77.5–122.5) | 120.6±7.5# | 115.7±8.2# | 121.8±10.1 | 112.7±9.1 |
| SLIS (mm) | |||||||
| Left | 42.0±11.0 (25.6–59.4) | 28.2±9.7 (10–35) | 35.5±4.6 (25.7–43.4) | 26.2±3.3 | 27.7±6.0 | – | – |
| Right | 43.0±12.0 (22.1–61.0) | 31.2±5.0 (26.0–41.3) | 33.9±5.3 (19–41.8) | 26.9±4.8 | 28.0±5.2 | – | – |
| IW (mm) | |||||||
| Left | – | – | 12.4±1.9 (10.4–17.3) | 17.0±3.5 | 14.8±2.5 | 18.1±3.4 | 15.9±2.8 |
| Right | – | – | 12.2±2.1 (7.5–16.9) | 17.0±2.8 | 14.9±2.6 | 18.5±3.7 | 16.0±3.1 |
| α (°) | |||||||
| Left | – | – | 38.4±5.5 (28.5–48.8) | 29.2±8.6 | 34.5±6.6 | 27.5±6.8 | 33.4±6.4 |
| Right | – | – | 39.0±5.0 (29.1–48.6) | 30.0±8.3 | 35.7± 7.5 | 28.0±7.2 | 33.9±6.6 |
| β (°) | |||||||
| Left | 46.0±10.8* (33.9–67.3) | 50.1±5.4* (43.8–58) | 38.9±3.3 (31.7–46.5) | 36.5±3.1 | 35.7±3.8 | 37.9±7.0 | 32.8±7.6 |
| Right | 52.2±5.4* (44.0–60.4) | 45.4±8.8* (32.0–57.0) | 40.8±6.1 (30.8–58.0) | 37.1±3.1 | 36.3± 3.3 | 37.7±7.5 | 32.4±7.1 |
| γ (°) | |||||||
| Left | 32.0±5.3 (21.6–40.0) | 29.4±7.7 (22.9–45.0) | – | – | – | – | – |
| Right | 34.6±6.6 (24.5–49.2) | 29.0±9.8 (19.0–46.2) | – | – | – | – | – |
#, the max length of screw trajectory; *, data calculated from its supplementary angle. S2AI, S2-alar-iliac; SL/STL, the screw length or screw trajectory length; SLIS, the screw length of the intrasacral part; IW, the iliac width defined as the narrowest iliac width measured between the inner cortices in the transverse plane; α, the angle between screw trajectory and horizontal line in the sagittal plane; β, the lateral trajectory angulation in the transverse plane; γ, the angle between screw trajectory and middle vertical line in the coronal plane.
Technique procedure
Reported mean values for iliac bone width range from 12.2–18.5 mm in different studies (12,13,17). Therefore, screws with diameter of 6.5 mm are suitable for most patients and 7.5 and 8.5 mm screws should also be well tolerated. The length of screw could be chosen from 65 to 120 mm depending on the specific anatomy of individuals.
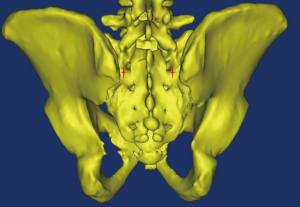
The optimal entry point of S2AI screw is located approximately 1 mm inferior and 1 mm lateral to the S1 dorsal foramen (11) (Figure 2), which is more medial and lower profile than iliac screw fixation. After determining the screw entry point, a drill or probe is used to fashion the screw trajectory (Figure 3), which can vary among individuals. Pre-operative screw trajectory measurements and intra-operative imaging may help optimize screw trajectory.
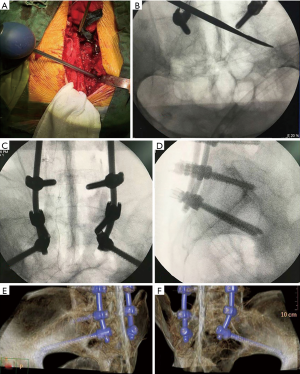
In 2015, Park et al. (18) reported the free hand S2AI insertion technique on cadaveric specimen. The midpoint between the S1 and S2 foramen and 2 mm medial to the lateral sacral crest was chosen as the entry point. After insertion of eight S2AI screws, visual and C-arm evaluation of the screw trajectory demonstrated accurate placement of all screws, with no violation of the sciatic notch, acetabulum, or pelvic cavity. The authors suggested that the free hand technique could reduce radiation exposure and surgical time.
Biomechanics
In 2013, O’Brien et al. (19) used seven human cadaveric spines to compare the biomechanical properties of 65-mm S2AI screws, 80-mm S2AI screws, and 90-mm iliac screws. The authors found that 65-mm S2AI screws were biomechanically equivalent to 80-mm S2AI screws and 90-mm iliac screws. Upon modification of S2AI screw fixation to penetrate through the posterior iliac cortex (quad-cortical S2AI screw fixation), no significant differences in biomechanical properties were demonstrated as compared to the previous fixation models. The cadaveric biomechanical study of Burns et al. (20) also found that the S2AI and iliac screws had similar biomechanical properties in regards to construct stiffness and failure. Hoernschemeyer et al. (21) found that S2AI screw fixation has a consistent trend towards increased construct stiffness, but was not statistically significant.
Another cadaveric biomechanical study conducted by Sutterlin et al. (22) compared five different models: L2-S1 pedicle screws fixation; L2-S1 pedicle screws fixation + S2AI screw fixation; L2-S1 pedicle screws fixation + L5/S1 TLIF (transforaminal lumbar interbody fixation); L2-S1 pedicle screws fixation + L5/S1 AxiaLIF (axial lumbar interbody fixation); and L2-S1 pedicle screws fixation + S2AI screw fixation + L5/S1 AxiaLIF. Strain gauges were placed on two S1 screws and one rod at the level of L5/S1. They found that the S2AI screws can reduce the strain on S1 screws during flexion-extension, lateral bending and axial torsion and can reduce rod strain during lateral bending and axial torsion as compared to AxiaLIF and interbody instrumentation models. However, this came at the expense of increased rod flexion-extension strain.
Preliminary clinical results
Sponseller et al. (23) reported on 32 consecutive pediatric patients who underwent S2AI screw fixation and found that the correction of pelvic obliquity and Cobb angles were 20°±11° (70%) and 42°±25° (67%), respectively. Compared to the 27 control patients who underwent spinal fusion and pelvic fixation with sacral or iliac screws, S2AI screw fixation demonstrated significantly better pelvic obliquity correction. Additionally, there were no vascular or neurologic complications, deep surgical site or wound infections reported in the S2AI group, and only four patients that developed superficial wound infections. In contrast, the control group developed three deep wound infections, and two instances of superficial wound infection or partial wound dehiscence. CT images obtained for 18 patients in the S2AI group showed no screw penetration into the pelvis, one screw tip with lateral protrusion (<5 mm), and one asymptomatic breakage of a 7-mm S2AI screw neck that did not require revision. Of note, one S2AI patient reported postoperative sacroiliac joint pain, requiring revision with longer screws bilaterally.
Mazur et al. (24) reported on 13 patients treated by S2AI screws fixation (26 S2AI screws), and found partial peri-screw lucency in 7 S2AI screws (27%) was found in 5 patients (38%), without major screw-related complications or sacroiliac joint degeneration. Mazur et al. (25) also used S2AI fixation in treatment of pyogenic vertebral diskitis and osteomyelitis at the lumbosacral junction. They suggested that S2AI fixation could provide rigid posterior fixation.
Ilyas et al. (26) compared S2AI to traditional iliac screw fixation and found S2AI screw fixation had decreased the rate of implant loosening, acute wound infections, delayed wound problems and revision surgery. A retrospective comparative study conducted by Elder et al. (27) also found that S2AI had lower rates of reoperation, surgical site infection, wound dehiscence and symptomatic screw prominence than iliac screw fixation. This study showed similar rates of pseudarthrosis, proximal junctional kyphosis and functional outcomes between S2AI versus iliac screw fixation. However, these studies are done retrospectively with short term follow up. Future prospective, long-term follow-up studies need to be conducted, with inclusion of joint penetration, and sacroiliac joint fusion or degeneration in outcome assessments (28,29).
Minimally invasive S2AI screw fixation
S2AI screws can also be inserted percutaneously. O’Brien et al. (14) performed percutaneous S2AI fixation on eight cadaveric spines, with visualization of the first dorsal foramen through standard anteroposterior and inlet radiographs, avoiding visceral or neurovascular structure injury. Martin et al. (30) also performed percutaneous S2AI screw fixation on two patients (a 69-year-old female with follicular thyroid carcinoma metastatic to the sacrum and a 55-year-old male with a sacral fracture), reporting minimal blood loss without intraoperative complications and immediate achievement of stability. El Dafrawy and Kebaish (31) reported on a 65-year-old woman who had an iliac stress fracture that progressed to nonunion. The authors performed the percutaneous S2AI screw fixation technique on her, with symptom relief reported at 2 months and radiographic union at 6 months. Funao et al. (32) additionally reported that the use of percutaneous of S2AI screw fixation was effective in the treatment of two cases of spondylodiscitis (one at L4-5, another at L5-S1). All these studies support that percutaneous S2AI screw fixation is a feasible and safe technique, with the added benefit of limited soft tissue damage.
Image-/robotic-guided S2AI screw fixation
Hu et al. (33) retrospectively reviewed the use of robotic guidance to insert 35 S2AI screws in 18 patients and reported no intra-operative complications with all screws demonstrating accurate trajectories on post-operative CT scans. To confirm the placement of the screws, the authors measured the distance between the pre-operative planned screws and post-operative inserted screws at two sites (one at the screw entry point, the other at the 30 mm depth point). They found that post-operative screws deviated from the pre-operative planned trajectories by 3.0±2.2 and 2.1±1.3 mm in the axial plane at the screw entry point and 30 mm depth point, respectively, and 1.8±1.6 and 1.2±1.1 mm in the lateral plane at the screw entry point and 30 mm depth point, respectively.
Bederman et al. (34) utilized robotic guidance to insert 31 S2AI screws and determined that all screws’ trajectories were placed accurately. Hyun et al. (35) also used robotic guidance to insert S2AI screws on four adult spinal deformity patients, and found that average surgical time was 13 min and 5.3 s of fluoroscopy per screw. All S2AI screws were placed accurately, without intra- or post-operative complications.
Image-/robotic-guided S2AI screw fixation can be performed by traditional open approach or minimally invasive approach. Current retrospective studies suggest that image-/robotic-guided S2AI screw fixation is a feasible and safe option for accurate screw placement.
Conclusions and key points
- The S2AI screw fixation is an anatomically feasible pelvic fixation technique, requiring less soft tissue dissection and avoiding instrumentation prominence;
- The S2AI screw entry point is approximately 1 mm inferior and 1 mm lateral to the S1 dorsal foramen;
- The diameter of S2AI screws ranges from 6.5 to 8.5 mm, and the length ranges from 65 to 120 mm;
- The S2AI screw can be inserted percutaneously or free handedly;
- There is no significant difference in biomechanical properties between S2AI and iliac screws;
- Retrospective, short-term outcomes reported in the literature show that S2AI has lower rates of reoperation, surgical site infection, wound dehiscence and symptomatic screw prominence than iliac screw fixation;
- Image or robotic guidance may provide a feasible and safe option for accurate screw placement.
Acknowledgements
Funding: This work was funded by the National Natural Science Foundation of China [81501933, 81572214], Wenzhou Leading Talent Innovative Projects (RX2016004), Wenzhou Municipal Science and Technology Bureau (Y20170389), Zhejiang Provincial Medical Technology Foundation of China under (2018KY129), Zhejiang Provincial Natural Science Foundation of China (LY14H060008). The funders had no role in the design, execution, or writing of the study.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.12.02). Dr. Wu serves as an unpaid Section Editor of AME Medical Journal. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mayer M, Stephan D, Resch H, et al. Biomechanical Comparison of Sacral Fixation Characteristics of Standard S1-Pedicle Screw Fixation versus a Novel Constrained S1-Dual-Screw Anchorage in the S1-Pedicle and S1-Alar Bone. Spine (Phila Pa 1976) 2015;40:1890-7. [Crossref] [PubMed]
- Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976) 2010;35:2245-51. [Crossref] [PubMed]
- Devlin VJ, Boachie-Adjei O, Bradford DS, et al. Treatment of adult spinal deformity with fusion to the sacrum using CD instrumentation. J Spinal Disord 1991;4:1-14. [PubMed]
- Dubory A, Bachy M, Bouloussa H, et al. Screw augmentation for spinopelvic fixation in neuromuscular spine deformities: technical note. Eur Spine J 2015;24:2580-7. [Crossref] [PubMed]
- Koller H, Zenner J, Hempfing A, et al. Reinforcement of lumbosacral instrumentation using S1-pedicle screws combined with S2-alar screws. Oper Orthop Traumatol 2013;25:294-314. [Crossref] [PubMed]
- Pham MH, Jakoi AM, Hsieh PC. S-1 and S-2-alar-iliac screw fixation via intraoperative navigation. Neurosurg Focus 2016;41 Video Suppl 1:1.
- Schwend RM, Sluyters R, Najdzionek J. The pylon concept of pelvic anchorage for spinal instrumentation in the human cadaver. Spine (Phila Pa 1976) 2003;28:542-7. [Crossref] [PubMed]
- Tsuchiya K, Bridwell KH, Kuklo TR, et al. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976) 2006;31:303-8. [Crossref] [PubMed]
- Kuklo TR, Bridwell KH, Lewis SJ, et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976) 2001;26:1976-83. [Crossref] [PubMed]
- Stevens DB, Beard C. Segmental spinal instrumentation for neuromuscular spinal deformity. Clin Orthop Relat Res 1989;164-8. [PubMed]
- O'Brien JR, Yu WD, Bhatnagar R, et al. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976) 2009;34:E439-42. [Crossref] [PubMed]
- Chang TL, Sponseller PD, Kebaish KM, et al. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976) 2009;34:436-40. [Crossref] [PubMed]
- Zhu F, Bao HD, Yuan S, et al. Posterior second sacral alar iliac screw insertion: anatomic study in a Chinese population. Eur Spine J 2013;22:1683-9. [Crossref] [PubMed]
- O'Brien JR, Matteini L, Yu WD, et al. Feasibility of minimally invasive sacropelvic fixation: percutaneous S2 alar iliac fixation. Spine (Phila Pa 1976) 2010;35:460-4. [Crossref] [PubMed]
- Wu AM, Chi YL, Ni WF, et al. The feasibility and radiological features of sacral alar iliac fixation in an adult population: a 3D imaging study. PeerJ 2016;4:e1587. [Crossref] [PubMed]
- Kwan MK, Jeffry A, Chan CY, et al. A radiological evaluation of the morphometry and safety of S1, S2 and S2-ilium screws in the Asian population using three dimensional computed tomography scan: an analysis of 180 pelvis. Surg Radiol Anat 2012;34:217-27. [Crossref] [PubMed]
- Yamada K, Higashi T, Kaneko K, et al. Optimal trajectory and insertion accuracy of sacral alar iliac screws. Acta Orthop Traumatol Turc 2017;51:313-8. [Crossref] [PubMed]
- Park JH, Hyun SJ, Kim KJ, et al. Free Hand Insertion Technique of S2 Sacral Alar-Iliac Screws for Spino-Pelvic Fixation: Technical Note, Acadaveric Study. J Korean Neurosurg Soc 2015;58:578-81. [Crossref] [PubMed]
- O'Brien JR, Yu W, Kaufman BE, et al. Biomechanical evaluation of S2 alar-iliac screws: effect of length and quad-cortical purchase as compared with iliac fixation. Spine (Phila Pa 1976) 2013;38:E1250-5. [Crossref] [PubMed]
- Burns CB, Dua K, Trasolini NA, et al. Biomechanical Comparison of Spinopelvic Fixation Constructs: Iliac Screw Versus S2-Alar-Iliac Screw. Spine Deform 2016;4:10-5. [Crossref] [PubMed]
- Hoernschemeyer DG, Pashuck TD, Pfeiffer FM. Analysis of the s2 alar-iliac screw as compared with the traditional iliac screw: does it increase stability with sacroiliac fixation of the spine? Spine J 2017;17:875-9. [Crossref] [PubMed]
- Sutterlin CE 3rd, Field A, Ferrara LA, et al. Range of motion, sacral screw and rod strain in long posterior spinal constructs: a biomechanical comparison between S2 alar iliac screws with traditional fixation strategies. J Spine Surg 2016;2:266-76. [Crossref] [PubMed]
- Sponseller PD, Zimmerman RM, Ko PS, et al. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine (Phila Pa 1976) 2010;35:1887-92. [Crossref] [PubMed]
- Mazur MD, Mahan MA, Shah LM, et al. Fate of S2-Alar-Iliac Screws After 12-Month Minimum Radiographic Follow-up: Preliminary Results. Neurosurgery 2017;80:67-72. [PubMed]
- Mazur MD, Ravindra VM, Dailey AT, et al. Rigid Posterior Lumbopelvic Fixation without Formal Debridement for Pyogenic Vertebral Diskitis and Osteomyelitis Involving the Lumbosacral Junction: Technical Report. Front Surg 2015;2:47. [Crossref] [PubMed]
- Ilyas H, Place H, Puryear A. A Comparison of Early Clinical and Radiographic Complications of Iliac Screw Fixation Versus S2 Alar Iliac (S2AI) Fixation in the Adult and Pediatric Populations. J Spinal Disord Tech 2015;28:E199-205. [Crossref] [PubMed]
- Elder BD, Ishida W, Lo SL, et al. Use of S2-Alar-iliac Screws Associated With Less Complications Than Iliac Screws in Adult Lumbosacropelvic Fixation. Spine (Phila Pa 1976) 2017;42:E142-9. [Crossref] [PubMed]
- Tseng C, Liu Z, Qiu Y, et al. Editorial on “Use of S2-alar-iliac screws associated with less complications than iliac screws in adult lumbosacropelvic fixation”. AME Med J 2017;2:56. [Crossref]
- Gupta S, Smith E, Falk D, et al. S2 alar-iliac screws versus iliac screws for pelvic fixation. AME Med J 2017;2:58. [Crossref]
- Martin CT, Witham TF, Kebaish KM. Sacropelvic fixation: two case reports of a new percutaneous technique. Spine (Phila Pa 1976) 2011;36:E618-21. [Crossref] [PubMed]
- El Dafrawy MH, Kebaish KM. Percutaneous S2 alar iliac fixation for pelvic insufficiency fracture. Orthopedics 2014;37:e1033-5. [Crossref] [PubMed]
- Funao H, Kebaish KM, Isogai N, et al. Utilization of a Technique of Percutaneous S2 Alar-Iliac Fixation in Immunocompromised Patients with Spondylodiscitis. World Neurosurg 2017;97:757 e11-8.
- Hu X, Lieberman IH. Robotic-guided sacro-pelvic fixation using S2 alar-iliac screws: feasibility and accuracy. Eur Spine J 2017;26:720-5. [Crossref] [PubMed]
- Bederman SS, Hahn P, Colin V, et al. Robotic Guidance for S2-Alar-Iliac Screws in Spinal Deformity Correction. Clin Spine Surg 2017;30:E49-53. [PubMed]
- Hyun SJ, Kim KJ, Jahng TA. S2 alar iliac screw placement under robotic guidance for adult spinal deformity patients: technical note. Eur Spine J 2017;26:2198-203. [Crossref] [PubMed]
Cite this article as: Wu AM, Chen D, Chen CH, Li YZ, Tang L, Phan K, Singh K, Haws BE, Vanni D, Mosley YI, Prasad SK, Harrop JS, Lin ZK, Lin Y, Ni WF, Wang XY; AME Spine Surgery Collaborative Group. The technique of S2-alar-iliac screw fixation: a literature review. AME Med J 2017;2:179.

