
Mixed hemangioma on the ileocecal valve removed by endoscopic polypectomy
Introduction
Gastrointestinal hemangiomas are uncommon benign vascular tumor occurring anywhere in the gastrointestinal tract and are usually seen in teenagers (1). A survey of 9,000 colonoscopies performed during a study period of 13 years has revealed only two cases of hemangiomas (2). Gastrointestinal hemangiomas are most commonly found in the small bowel followed by the colon. Gastrointestinal hemangiomas are divided into three types: the first type, the capillary hemangioma, described as a small tuft of sub-mucosal capillaries that expand intraluminally and may develop into a skalk-like mass; the second type, represented by mixed capillary and cavernous hemangioma; the third and the most common type, which is the cavernous hemangioma (3). Diagnosis and therapy are typically delayed due to low clinical suspicion. Phlebolith is a pathognomonic finding which might be observed in 26–50% of the patients’ abdominal radiographs. The abdominal computer tomography (CT) may reveal thickened colonic wall and pelvic phleboliths. Colonoscopy is essential for the diagnosis of hemangiomas in colon. In this report, we describe a case of mixed hemangioma in an old woman treated at our hospital.
Case presentation
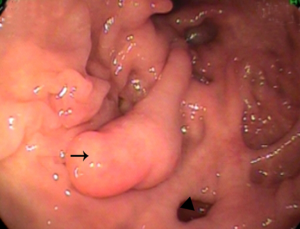
A 74-year-old woman presented with abdominal pain and diarrhea. She underwent colonoscopy in another hospital and colonoscopy revealed multiple polyps and diverticula in the cecum. So she was referred to our hospital for polypectomy. She mentioned a chronic pain over her periumbilicus and diarrhea with watery stool for three months. She has history of hypertension under medication control. She had no symptom of vomiting, melena, fever, or weight loss. Laboratory study, chest X-ray and abdominal ultrasonography were unremarkable. During the colonoscopy we found multiple polyps and diverticula in the cecum (Figure 1, arrowhead). A pedunculated polypoid mass on the ileocecal valve with a diameter of 15 mm was noted (Figure 1, arrow). The mass had a long stalk and was not ulcerated. The mass had smooth surface with the same color as the surrounding mucosa and was elastic and compressible. The mass was successfully removed by snare polypectomy and send to pathological department for histological examination. There was no complication such as bleeding and perforation. And the patient recovered uneventfully.
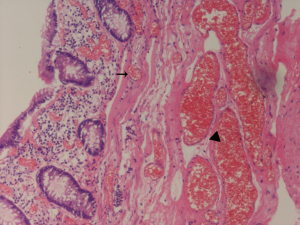
Photomicrograph shows normal colonic mucosa at the surface of the mass. There are numerous thin-walled capillaries lined with endothelial cells in submucosa tissue (Figure 2, arrow). And the proliferation of large blood-filled spaces in submucosa tissue was also noted (Figure 2, arrowhead). Photomicrograph shows blood-filled vessels throughout submucosa. The diagnosis of mixed hemangioma on the ileocecal valve was decided.
Discussion
Hemangiomas are congenital, benign, vascular lesions and may become symptomatic decades later. The lesions are venous malformation and not true tumors. Phillips reported the first case of rectal hemangioma in 1839 (4). The most common site of gastrointestinal hemangiomas is the small intestine and hemangiomas of the colon are rare, with the rectosigmoid being the most commonly involved part. Hemangiomas of colon are of clinical importance due to the possibility of massive bleeding (5-7). Histologically, most colorectal hemangiomas are capillary or cavernous and mixed hemangiomas are rare in colon. Capillary hemangiomas consist of a proliferation of small capillaries composed of thin-walled spaces lined by endothelial cells, while cavernous hemangiomas are composed of numerous dilated, thin-walled, irregular blood-filled spaces mainly located within the mucosa and submucosa, sometimes extending through the muscular layer to the serosa (8,9). Approximately 50% of all reported colonic hemangiomas have been described as the cavernous type. Capillary hemangiomas of the colon are often asymptomatic, but cavernous tumors frequently bleed briskly early in life. Patients mainly present with painless bleeding and more than half of the patients have some degree of iron deficiency anemia, but they can also present with abdominal pain, mechanical bowel obstruction, or perforation (10).
Over 200 cases of colonic hemangioma have been reported. It is very important to recognize hemangiomas in order to adopt the most appropriate treatment. It is relatively easy to diagnose the typical hemangioma presenting as translucent blue-purple vessels under the mucosa. But some hemangiomas are diagnosed difficulty due to their atypical shape and color and to lack of knowledge. Oner and Altaca reported an average delay of 19 years between the appearance of the initial symptoms and diagnosis (11). A number of patients with gastrointestinal hemangiomas were misdiagnosed and underwent unnecessary intervention (12). Internal hemorrhoids, carcinoma, adenomatous polyps and ulcerative colitis are the main mimicking lesions that have been reported (13). Endoscopy, plain X-ray of abdomen, barium contrast study, CT, MRI and angiography are useful measurements of investigation for accurate diagnosis. Endoscopy is essential for the diagnosis and hemangiomas are typically red, purple, or bluish nodules or dilated vessels. Hemangiomas may present as a pedunculated, subpedunculated, or flat elevated lesion similar to polyp or submucosal tumor. Most lesions are soft and compressible. The hemangiomas in gastrointestinal tract can be solitary or clusters of lesions (14,15), or part of a more complex syndrome with cutaneous manifestations (2). These lesions should not be biopsied due to the risk of bleeding, therefore obtaining the histological diagnosis of hemangioma before treatment is difficult. Colonoscopy plays role in the diagnosis of colon hemangiomas and may be potentially therapeutic. On plain film of the abdomen, the visualization of phleboliths is an important diagnostic criterion, that is observed in 26–50% of adult patients, but their absence does not exclude the diagnosis (16). Double contrast barium study can demonstrate nodular defect, which may change configuration after compression (17). CT scan can show transmural thickening of the intestinal wall and identify the phleboliths. Magnetic resonance can reveal wall thickening of intestine and demonstrate heterogeneous bright signal intensity on T2-weighted images. Angiography demonstrates mural hypervascularity with delayed venous pooling but is rarely necessary to establish the diagnosis. Some cases are diagnosed after the lesions are resected. A polypoid hemangioma in colon was a rare disease (14,18) and there is no report about a hemangioma on the ileocecal valve.
Most hemangiomas have been resected surgically and with the improvement of endoscopic techniques some hemangiomas have been treated with endoscopy successfully (19). Endoscopic therapy is mildly invasive compared with surgical resection. As for solitary, pedunculated and small polypoid hemangiomas in gastrointestinal tract endoscopic resection is reasonable choice because of its safety and low cost. The methods of endoscopic therapy for hemangiomas in gastrointestinal tract include cyanoacrylate glue injection (20), endoscopic mucosa resection (EMR) (19), argon plasma coagulation and polypectomy (18). Kimura advocated performing endoscopic ultrasound (EUS) before endoscopic treatment for gastrointestinal hemangiomas to avoid treating lesions with transmural involvement. For larger, multiple or diffuse hemangiomas surgical treatment is the first choice. Angiography is another potentially therapeutic technique that can be used alone or in combination with surgical resection.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.12.04). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pohlen U, Kroesen AJ, Berger G, et al. Diagnostic and surgical treatment strategy for rectal cavernous hemangiomas based on three case examples. Int J Colorectal Dis 1999;14:300-3. [Crossref] [PubMed]
- Topalak O, Gönen C, Obuz F, Secil M. Diffuse cavernous hemangioma of the rectosigmoid colon with extraintestinal involvement. Turk J Gastroenterol 2006;17:308-12. [PubMed]
- Enziger FM, Weiss SW. Soft tissue tumors. 3rd ed. St. Louis, Mossouri: Mosby-Yearbook, 1995:679-89.
- Phillips B. Rectile tumor of the anus. Lond Med Gaz 1839;23:514-9.
- Varma JD, Hill MC, Harvey LA. Hemangioma of the small intestine manifesting as gastrointestinal bleeding. Radiographics 1998;18:1029-33. [Crossref] [PubMed]
- Pontecorvo C, Lombardi S, Mottola L, et al. Hemangioma of the large bowel. Report of a case. Dis Colon Rectum 1983;26:818-20. [Crossref] [PubMed]
- Hasegawa K, Lee WY, Noguchi T, et al. Colonoscopic removal of hemangiomas. Dis Colon Rectum 1981;24:85-9. [Crossref] [PubMed]
- Levy AD, Abbott RM, Rohrmann CA Jr, et al. Gastrointestinal hemangiomas: imaging findings with pathologic correlation in pediatric and adult patients. AJR Am J Roentgenol 2001;177:1073-81. [Crossref] [PubMed]
- Greenwald DA, Brandt LJ. Vascular lesions of the gastrointestinal tract. In: Feldman M, Friedman LS, Sleisenger MH, eds. Sleisenger & Fordtran’s Gastrointestinal and liver disease. Pathophysiology/Diagnosis/Management. 7th ed. Philadelphia: Saunders, 2002:2341-55.
- Demirbas T, Güler N, Caliskan C, et al. Mechanical bowel obstruction due to colonic hemangioma: Report of a case. Turk J Gastroenterol 2006;17:305-7. [PubMed]
- Oner Z, Altaca G. Diffuse cavernous rectal hemangioma—clinical appearance, diagnostic modalities and sphincter saving approach to therapy: report of 2 and a collective review of 79 cases. Acta Chir Belg 1993;93:173-6. [PubMed]
- Tan TC, Wang JY, Cheung YC, et al. Diffuse cavernous hemangioma of the rectum complicated by invasion of pelvic structures. Report of two cases. Dis Colon Rectum 1998;41:1062-6. [Crossref] [PubMed]
- Hsu RM, Horton KM, Fishman EK. Diffuse cavernous hemangiomatosis of the colon: findings on three-dimensional CT colonography. AJR Am J Roentgenol 2002;179:1042-4. [Crossref] [PubMed]
- Yorozuya K, Watanabe M, Hasegawa H, et al. Diffuse cavernous hemangioma of the rectum: report of a case. Surg Today 2003;33:309-11. [Crossref] [PubMed]
- Dobozi BM, Rockey DC. Diffuse colonic hemangiomatosis. Gastrointest Endosc 2004;60:799. [Crossref] [PubMed]
- Tanaka N, Onda M, Seya T. Diffuse cavernous hemangioma of the rectum. Eur J Surg 1999;165:280-3. [Crossref] [PubMed]
- Dachman AH, Ros PR, Shekikta KM, et al. Colorectal hemangioma: radiologic findings. Radiology 1988;167:31-4. [Crossref] [PubMed]
- van Deursen1 CT, Buijs1 J, Nap M. An uncommon polyp in the colon: a pedunculated cavernous hemangioma. Endoscopy 2008;40:E127 [Crossref] [PubMed]
- Kimura S, Tanaka S, Kusunoki H, et al. Cavernous hemangioma in the ascending colon treated by endoscopic mucosal resection. J Gastroenterol Hepatol 2007;22:280-1. [Crossref] [PubMed]
- Zurakowski J, Swiercz P, Wróblewski T, et al. Diffuse cavernous hemangiomas of rectosigmoid colon treated with n-butyl-2-cyanoacrylate injections. Endoscopy 2008;40:E120-1. [Crossref] [PubMed]
Cite this article as: Shao XD, Guo XZ, Ren LN, Liang ZD. Mixed hemangioma on the ileocecal valve removed by endoscopic polypectomy. AME Med J 2018;3:12.

