
A biomechanical analysis of intramedullary nailing for humeral shaft fractures using 3D-finite element method
Introduction
It is widely accepted that acute fractures of the humerus have a good healing tendency by conservative treatment, because of an excellent blood supply to the bony fragments by the surrounding muscles (1-4). Conservative treatment, however, has limitations in cases of radial nerve palsy, extensive soft-tissue injury, multiple fractures, delayed union or nonunion, non-compliance or obesity (5,6). Plate osteosynthesis has been the treatment of choice when surgical procedure is needed (7,8).
Humeral locking nails were introduced to reproduce the success seen with similar devices used in the lower extremities. Even though advantages of interlocking nails compared with plating included less soft tissue damage, closed reduction and periosteum-sparing stabilization of complex fractures, these theoretical advantages were not confirmed and severe complications such as shoulder pain, delayed union, non-union and iatrogenic fractures were reported (5). Meanwhile, the decision on whether an antegrade or retrograde nailing is performed was left to the discretion of the surgeon (9). Authors reported that healing of acute humeral shaft fractures was not correlated to the direction of nailing (10,11), but in our experience, fracture healing was dependent upon choice of nail insertion according to the fracture sites of the humerus. In addition, to the knowledge of the authors no clinical and biomechanical results have been regarding the bone healing on the direction of interlocking nailing in the proximal, midshaft and distal diaphysis of the humerus. Hence the purpose of this study was to analyze the biomechanical properties of antegrade and retrograde nailing under three types of loads [axial compression, anterior-posterior (AP) bending and torsion] in diaphyseal fractures according to levels of the humerus.
Methods
Based on the geometrical configurations and Unreamed Humeral Nails and CT scans of the humerus, 3D geometrical and finite element method (FEM) models of antegrade and retrograde nailing with humeral shaft fractures were formed by using Solidworks software. With ANSYS 15.0 program, the model was meshed into 6,042 pieces of parabolic tetrahedron elements. By combining these models, interlocking nailing of the humeral shaft fracture was modeled, which consisted of fractured humerus, intramedullary nail and interlocking screws. The mechanical values which were inputted to this FEM model are as follows (Table 1).
Table 1
| Compartment | Young’s modulus (Kgf/cm2) | Poisson ratio |
|---|---|---|
| Humerus | 17,000 | 0.30 |
| Nickel | 2,100,000 | 0.31 |
To conduct finite element analysis, it was supposed that antegrade and retrograde nailing with double interlocking screws insertion in each fragment was undergone respectively in the proximal, distal shaft and midshaft of the humerus of a person; 39 years old, 1.72 m tall and 60 kg weighted.
While the proximal end of the humerus was being constrained, bending force was applied to the fracture site by 5 N, for torsional testing, rotational moment of 0.1 Nm was applied to the distal end of the humerus and axial compression was transmitted through the distal end by 100 N.
According to antegrade and retrograde technique, values of stiffness and displacement at the fracture sites and the humerus were obtained.
Results
Bending properties
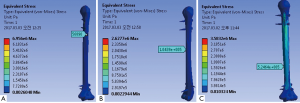
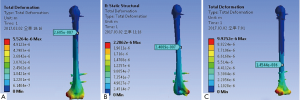
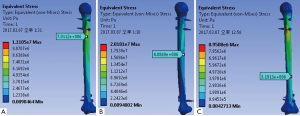
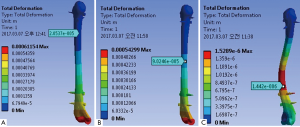
During the testing under AP bending, the values of stiffness (Figures 1,2) and displacement (Figures 3,4) at the fracture site and the humerus are as follows (Table 2).
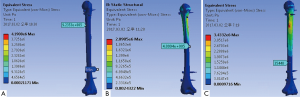
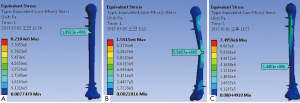
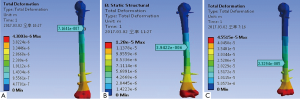

Table 2
| Biomechanical properties | Antegrade technique (fracture site) | Retrograde technique (fracture site) | |||||
|---|---|---|---|---|---|---|---|
| Proximal diaphysis | Midshaft | Distal diaphysis | Proximal diaphysis | Midshaft | Distal diaphysis | ||
| Displacements at the fracture site (m) | 7.164×10–7 | 3.9422×10–6 | 2.329×10–5 | 1.8934×10–4 | 1.6254×10–6 | 3.1552×10–5 | |
| Fracture stiffness (Pa) | 9.235×105 | 4.099×105 | 35,440 | 1.0923×106 | 5.5027×105 | 1.4451×106 | |
| Maximum stiffness (Pa) | 4.19×106 | 2.098×106 | 3.433×106 | 8.218×106 | 1.5515×106 | 7.4959×106 | |
| Minimum stiffness (Pa) | 0.00021 | 0.00024 | 0.00097 | 0.0077 | 0.00218 | 0.0004 | |
| Maximum displacements (m) | 4.3×10–6 | 1.28×10–5 | 4.55×10–5 | 0.00092 | 1.6298×10–6 | 6.2824×10–5 | |
| Minimum displacements (m) | 4.778×10–7 | 1.4223×10–6 | 5.057×10–6 | 0.0001 | 1.8×10–7 | 6.98×10–6 | |
Compared values of fracture bending stiffness by antegrade nailing with those by retrograde nailing according to fracture levels under bending force, the value of antegrade technique in proximal shaft was lower than the value of retrograde. Also, antegrade nailing demonstrated less stiffness than retrograde nailing, but the difference was not found to be great. In addition to the values of fracture bending stiffness, maximum stiffness values of the humerus had a similar tendency to those.
From the viewpoint of displacement, the value of fracture site produced in antegrade approach by bending force was considerably lower than the value in retrograde nailing in the proximal diaphysis. Displacements in the midshaft and distal diaphysis were not different between the nailing directions. Maximum and minimum values of the humerus were found to be as well as the values of fracture site.
Torsional properties
Table 3 presents the results of testing under torsion.
Table 3
| Biomechanical properties | Antegrade technique (fracture site) | Retrograde technique (fracture site) | |||||
|---|---|---|---|---|---|---|---|
| Proximal diaphysis | Midshaft | Distal diaphysis | Proximal diaphysis | Midshaft | Distal diaphysis | ||
| Displacements at the fracture site (m) | 2.685×10–7 | 3.4×10–7 | 1.4544×10–6 | 3.1596×10–5 | 1.578×10–7 | 1.3952×10–5 | |
| Fracture stiffness (Pa) | 5.321×105 | 7.5429×105 | 5.97×105 | 56890 | 1.044×105 | 5.246×105 | |
| Maximum stiffness (Pa) | 3.3759×106 | 1.303×106 | 3. 8833×106 | 6.956×106 | 2.627×106 | 3.583×106 | |
| Minimum stiffness (Pa) | 0.0115 | 0.0126 | 0.0259 | 0.0026 | 0.00229 | 0.0103 | |
| Maximum displacements (m) | 5.5264×10–6 | 2.2062×10–6 | 9.925×10–6 | 0.0004 | 1.267×10–6 | 5.648×10–6 | |
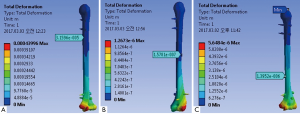
The values of fracture torsional stiffness in antegrade nailing in the proximal, distal diaphysis and midshaft were somewhat greater than in retrograde technique, but the maximum values were not great on the contrary (Figures 5,6).
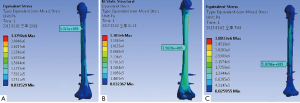
Antegrade nailing resulted in less displacements of fractures site during torsional testing in the proximal and distal diaphysis than retrograde nailing (Figures 7,8).
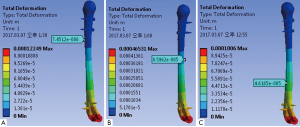
Axial compression properties
As described in the Table 4, in the distal shaft, the value of fracture site stiffness by antegrade nailing under axial compression was lower than the value by retrograde technique. Also, retrograde nailing showed less stiffness than antegrade nailing in the proximal diaphysis and midshaft, but there was no significant difference between them. Maximum stiffness values of antegrade nailing in the proximal, distal diaphysis and midshaft were lower than retrograde nailing (Figures 9,10).
Table 4
| Biomechanical properties | Antegrade technique (fracture site) | Retrograde technique (fracture site) | |||||
|---|---|---|---|---|---|---|---|
| Proximal diaphysis | Midshaft | Distal diaphysis | Proximal diaphysis | Midshaft | Distal diaphysis | ||
| Displacements at the fracture site (m) | 2.05×10–5 | 9.02×10–5 | 1.442×10–6 | 7.4512×10–6 | 8.5962×10–5 | 4.617×10–5 | |
| Fracture stiffness (Pa) | 7.84×106 | 4.26×106 | 2.69×105 | 7×106 | 4.1×106 | 3.19×106 | |
| Maximum stiffness (Pa) | 1.085×107 | 6.45×106 | 6×106 | 1.11×107 | 2×107 | 8.95×106 | |
| Minimum stiffness (Pa) | 0.0419 | 0.0341 | 0.0012 | 0.009 | 0.0094 | 0.0042 | |
| Maximum displacements (m) | 6.115×10–4 | 5.43×10–4 | 1.53×10–6 | 1.229×10–4 | 4.653×10–4 | 1×10–4 | |
| Minimum displacements (m) | 6.79×10–5 | 6×10–5 | 1.7×10–7 | 1.36×10–6 | 5.17×10–5 | 1.178×10–5 | |
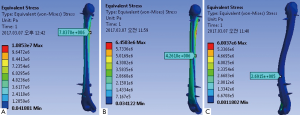
Displacements of fracture site and maximum displacements had a similar tendency to the stiffness on axial compression (Figures 11,12).
Discussion
Conservative treatment is indicated in undisplaced fractures, if patients refuse operative stabilization and in patients with indication for surgery. Plating is frequently used for metaphyseal fractures or fractures with an extension into the joint. External fixation is seldom used. The main indications are severe soft tissue injuries, severe contamination and infection (12,13). After soft tissue healing, conversion to definitive internal fixation is planned (14).
Double interlocking on either fragment of the fracture provides higher axial and rotator stability than single interlocking. Interlocking through slots is less stable than through round static holes (15).
The choice of an antegrade or retrograde approach was dependent on the preference of the surgeon. Healing of acute humeral shaft fractures is independent of the direction of nailing (10,11).
In our experience, however, fracture healing was different between antegrade and retrograde nailing according to the fracture levels. For example, a patient with the distal shaft fracture of the humerus was operated with a retrograde nailing, which resulted in nonunion after 6 months and reoperated with a plate osteosynthesis (Figure 13). Hence, we purposed to analyze the biomechanical properties of antegrade and retrograde nailing under three types of loads (axial compression, AP bending and torsion) in diaphyseal fractures according to the levels of the humerus.

In our study we formed 3D geometrical and FEM models of the humeral fractures and intramedullary nails using Solidworks software and analyzed biomechanical properties of humeral nailing under 3 types of loads: AP bending, torsion and axial compression with ANSYS 15.0 program. To estimate and compare biomechanical stability of antegrade and retrograde nailing, were formed using Solidworks software based on CT scans of the humerus and analyzed with ANSYS 15.0 program. Biomechanical analysis was performed under three types of loads: AP bending, torsion and axial compression.
During the bending test, values of fracture stiffness by antegrade nailing were lower than those by retrograde nailing in proximal, distal diaphysis and midshaft. The displacement of fracture site in the proximal diaphysis by antegrade approach was considerably lower than in retrograde nailing, while displacements in the midshaft and distal diaphysis were not different between the nailing directions. This means that antegrade nailing is safer than retrograde nailing on the bending force, especially in the proximal diaphysis.
Under torsional load, the values of fracture stiffness in antegrade nailing in the proximal, distal diaphysis and midshaft were somewhat greater than in retrograde technique, but the maximum values were not great on the contrary. Antegrade nailing resulted in less displacements of fractures site in the proximal and distal diaphysis than retrograde nailing. On torsional load, antegrade nailing was found to be more stable than retrograde nailing in the proximal and distal diaphysis.
As applied axial compression, in the distal shaft, the value of fracture site stiffness by antegrade nailing was lower than the value by retrograde technique. Also, retrograde nailing showed less stiffness than antegrade nailing, but there was no significant difference between them. Displacements of fracture site and maximum displacements showed a similar tendency to the stiffness on axial compression. It is shown that under axial compression in the distal diaphysis, antegrade nailing is a safer procedure compared to retrograde approach.
Conclusions
Humeral nailing can be used by either antegrade or retrograde technique and its insertion direction may be dependent upon the preference of the surgeon. According to the levels of fracture in the humerus, however, antegrade and retrograde nailing produces different stabilities. In the proximal and distal diaphysis, antegrade nailing is a safer procedure than retrograde nailing biomechanically. There is no difference between antegrade and retrograde technique in the midshaft fracture.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2019.09.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This article does not contain any studies with human participants or animals performed by any of the authors.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Böhler L. Gegen die operative Behandlung von frischen Oberarmschaftbrüchen. Langenbecks Arch Surg 1964;308:465-70. [Crossref]
- Sarmiento A, Kinman PB, Galvin EG, et al. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am 1977;59:596-601. [Crossref] [PubMed]
- Wallny T, Westermann K, Sagebiel C, et al. Functional treatment of humeral shaft fractures: indications and results. J Orthop Trauma 1997;11:283-7. [Crossref] [PubMed]
- Zagorski JB, Latta LL, Zych GA, et al. Diaphyseal fractures of the humerus. Treatment with prefabricated braces. J Bone Joint Surg Am 1988;70:607-10. [Crossref] [PubMed]
- Farragos AF, Schemitsch EH, McKee MD. Complications of intramedullary nailing for fractures of the humeral shaft: a review. J Orthop Trauma 1999;13:258-67. [Crossref] [PubMed]
- Holm CL. Management of humeral shaft fractures. Fundamental nonoperative technics. Clin Orthop Relat Res 1970;132-9. [PubMed]
- Bell MJ, Beauchamp CG, Kellam JK, et al. The results of plating humeral shaft fractures in patients with multiple injuries. The Sunnybrook experience. J Bone Joint Surg Br 1985;67:293-6. [Crossref] [PubMed]
- Heim D, Herkert F, Hess P, et al. Surgical treatment of humeral shaft fractures--the Basel experience. J Trauma 1993;35:226-32. [Crossref] [PubMed]
- Rommens PM, Kuechle R, Bord T, et al. Humeral nailing revisited. Injury 2008;39:1319-28. [Crossref] [PubMed]
- Blum J, Rommens PM, Janzing H, et al. Unfallchirurg 1998;101:342-52. [Retrograde nailing of humerus shaft fractures with the unreamed humerus nail An international multicenter study]. [Crossref] [PubMed]
- Blum J, Janzing H, Gahr R, et al. Clinical performance of a new medullary humeral nail: antegrade versus retrograde insertion. J Orthop Trauma 2001;15:342-9. [Crossref] [PubMed]
- Smith DK, Cooney WP. External fixation of high-energy upper extremity injuries. J Orthop Trauma 1990;4:7-18. [Crossref] [PubMed]
- Zinman C, Norman D, Hamoud K, et al. External fixation for severe open fractures of the humerus caused by missiles. J Orthop Trauma 1997;11:536-9. [Crossref] [PubMed]
- Dougherty PJ, Silverton C, Yeni Y, et al. Conversion from temporary external fixation to definitive fixation: shaft fractures. J Am Acad Orthop Surg 2006;14:S124-7. [Crossref] [PubMed]
- Blum J, Machemer H, Baumgart F, et al. Biomechanical comparison of bending and torsional properties in retrograde intramedullary nailing of humeral shaft fractures. J Orthop Trauma 1999;13:344-50. [Crossref] [PubMed]
Cite this article as: Ko MS, Kang GR, Kim JS, Pak HN, Choe GR, Ra JM. A biomechanical analysis of intramedullary nailing for humeral shaft fractures using 3D-finite element method. AME Med J 2019;4:36.

