
Performance of short type double balloon enteroscope in endoscopic retrograde cholangiopancreatography: does the length of a scope matter?—a systematic review and meta-analysis
Introduction
Since the first report of endoscopic retrograde cholangiopancreatography (ERCP) in 1968, this endoscopic intervention has been widely used to diagnose and treat pancreaticobiliary diseases (1). The reported success rate of diagnostic and therapeutic ERCP in patients with normal anatomy is 90–95% (2,3). ERCP has been commonly used as the initial attempt to treat postoperative disorders prior to percutaneous approach and reoperation. ERCP in patients with previous surgery and reconstruction of gastrointestinal tract is often challenging. Success rate of ERCP in patients with surgically altered anatomy is lower than that in patients with normal anatomy (4). The conventional scopes, including duodenoscope, gastroscope and colonoscope, cannot reach the papilla or surgical anastomosis in some patients. The success rates of ERCP in patients with surgically altered anatomy using these conventional scopes are 50–92% (5-12). The causes of the difficulty of ERCP in patients with gastrointestinal tract reconstruction include difficulty in inserting an endoscope into the target site, in cannulating selectively into biliary/pancreatic duct, and in completing desired therapeutic procedures safely. The angulation of various anastomoses and the adhesions make cannulation and other endoscopic interventions more difficult. As a result, many of these patients are referred to percutaneous or surgical interventions which are more invasive than endoscopic therapy (13). The adverse event rates of percutaneous transhepatic cholangiography (PTC) for postoperative biliary stricture are between 11–35%, including hepatic artery injury, post-procedure sepsis, and hepatic abscess (14). PTC is not feasible in patients with ascites and coagulopathy and has low success rate in patients without obvious dilated intrahepatic duct. In addition, PTC cannot deal with disorders in pancreatic duct. Open surgery is often technically difficult and associated with more complications, and requires long-term hospitalization.
Eighteen years ago, double balloon enteroscope (DBE) was available in clinical practice which allowed the access to pancreaticobiliary limb of small intestine in patients with surgically altered anatomy (15-18). Taking advantage of the balloons attached to the tip of the scope and overtube, DBE increases the possibility of accessing to the papilla or pancreaticobiliary anastomosis and makes cannulation of biliary/pancreatic duct possible (19-21). The invention of DBE has dramatically changed the endoscopic management of pancreaticobiliary disease in patients with surgically altered anatomy. Some studies had confirmed that ERCP assisted with DBE (DBE-ERCP) is an effective method for interventions in the pancreaticobiliary system in the postoperative patients (22-25). The superiority of DBE compared with conventional endoscopes in the treatment of pancreaticobiliary disease in patients with surgically altered anatomy was reported in several studies (26-29). In the beginning DBE-ERCP was performed with the conventional long DBE (200 cm) the length of which precluded the use of standard ERCP accessories (30,31). The lack of adequate accessories makes pancreaticobiliary interventions difficult and time-consuming. The gastrointestinal tract reconstructions for which ERCP is carried out with DBE mainly include Roux-en-Y reconstruction, pancreatoduodenectomy (PD), and Billroth II gastrectomy. It is still difficult, however, not only to reach the target site, but also to cannulate selectively into biliary/pancreatic duct during DBE-ERCP in some patients. Therefore, innovation of endoscope has been required to improve the outcome of DBE-ERCP. A short type DBE (sDBE) has been developed to allow use of standard ERCP accessories. Numerous reports of ERCP with sDBE (sDBE-ERCP) have been published since 2009 and reported overall ERCP success rates varying widely (32-45). Previous studies of sDBE-ERCP have reported success rates of reaching the target site of 86–100%, success rates of ERCP-related interventions of 90–96%, and overall success rates of 81–94% (18,25,39,46). Most of these studies were retrospective and had small sample size. There have been no systematic reviews or meta-analyses of this method until now. We performed a systematic review and meta-analysis to evaluate the efficacy and safety of sDBE-ERCP in patients with surgically altered anatomy.
Methods
Literature search
A comprehensive literature search was conducted using PubMed, EMBASE, and Cochrane Library for the period from January 2001 to December 2018. The search terms were: “endoscopic retrograde cholangiopancreatography” or “ERCP” or “endoscopic retrograde cholangiography” or “endoscopic retrograde pancreatography” and “double balloon enteroscope” or “balloon-assisted enteroscope”. The search was limited to studies in humans published in English. References of eligible articles and review articles were manually searched.
Selection of articles
The selection criteria were studies in (I) patients with surgically altered anatomy; (II) patients undergoing sDBE-ERCP due to pancreaticobiliary problems; and (III) series that included at least 10 patients. Case reports or series with fewer than 10 patients were excluded. After excluding duplicate articles, article titles and abstracts were screened by a reviewer (SXD). Each eligible article was reviewed in full text.
Data extraction
Data were abstracted by the same reviewer and entered into an Excel spreadsheet (Microsoft Corp, Redmond, Washington). The following information were abstracted from each study: author, region, publication year, publication type, study design, participants, indication of ERCP, and outcome of interest (success rate of enteroscopy, success rate of diagnostic ERCP, success rate of therapeutic ERCP, overall success rate of ERCP, duration of procedure, and procedure-related complications).
Definitions
Success of enteroscopy: the pancreaticobiliary limb and papilla or bilioenteric/pancreaticoenteric anastomoses were successfully reached by using sDBE.
Success of diagnostic ERCP: selected cannulation into bile duct or pancreatic duct was achieved and cholangiogram or pancreatogram was clearly presented resulting in a diagnosis.
Success of therapeutic ERCP: intended endoscopic interventions were successfully performed by using sDBE-ERCP including sphincterotomy, balloon dilation for pancreaticobiliary duct stricture, pancreaticobiliary stones retrieval, biliary drainage, pancreatic drainage, and stent removal.
sDBE-ERCP-related complications: sDBE-ERCP-related complications include pancreatitis, perforation, cholangitis, bleeding, and other adverse events, which need further specific treatment.
Statistical analysis
Data from eligible studies were pooled using a random-effects model with StatsDirect statistical software Version 2.7.8 (StatsDirect Ltd, Sale, Cheshire, UK). Outcomes are expressed as proportions (percentages) with 95% confidence intervals (CIs). The pooled analyses are presented as forest plots. Statistical heterogeneity between studies was assessed using the Cochran Q test and the I2 statistic. An I2 value of greater than 50% or a P value of less than 0.05 for the Q statistic was taken to indicate significant heterogeneity. Three subgroup analyses of patients with Roux-en-Y reconstruction, patients with PD and patients with Billroth II gastrectomy were also performed.
Results
Literature search results
Nine studies involving a total of 1,054 procedures in 890 patients were included in the analysis. All studies were retrospective and published between 2009 and 2018. Six studies were excluded because each had a small number of study subjects (less than 10). Figure 1 summarizes the results of the literature search. Table 1 summarizes the characteristics of the 9 eligible studies.
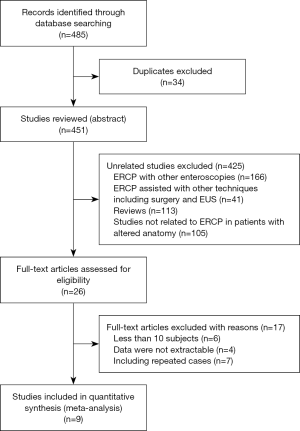
Table 1
| Author | Publication year | Regions | Publication type | Study design | No. cases | Age (years) | Gender (male) | Removal of stent | SOD | Pancreatic duct dilation | Biliary stone | Biliary stricture | Others |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shimatani et al. | 2009 | Japan | Full text | Retrospectively | 68 | NA | NA | NA | NA | NA | NA | NA | NA |
| Osoegawa et al. | 2012 | Japan | Full text | Retrospectively | 28 | 74.0 [54–91] | 18 | NA | NA | NA | NA | NA | NA |
| Siddiqui et al. | 2013 | USA | Full text | Retrospectively | 79 | 58 [29–86] | 30 | 5 | 3 | 2 | 48 | 18 | 0 |
| Choi et al. | 2013 | USA | Full text | Retrospectively | 28 | 56.1±12.2 | 2 | 0 | 6 | 0 | 16 | 4 | 2 |
| Tsutsumi et al. | 2014 | Japan | Full text | Retrospectively | 72 | 69 [37–83] | 44 | 0 | 0 | 0 | 0 | 72 | 0 |
| Tsou et al. | 2015 | Taiwan | Full text | Retrospectively | 47 | 54.4 [26–87] | 22 | 0 | 0 | 0 | 35 | 12 | 0 |
| Tomoda et al. | 2016 | Japan | Full text | Retrospectively | 20 | 55 [5–74] | 13 | 0 | 0 | 0 | 0 | 20 | 0 |
| Shimatani et al. | 2017 | Japan | Abstract | Retrospectively | 222 | NA | NA | NA | NA | NA | NA | NA | NA |
| Yamada et al. | 2018 | Japan | Full text | Retrospectively | 326 | NA | NA | 0 | 0 | 0 | 149 | 185 | 11 |
SOD, sphincter of Oddi dysfunction; NA, not applicable.
Characteristics of study
In the 9 studies, a total of 890 patients underwent 1,054 sDBE-ERCP procedures. All studies were retrospective and conducted between 2009 and 2018. Six studies were performed in Japan, followed by the United States (2/9) and Taiwan (1/9). The largest report included 326 patients and all papers included more than 20 patients. The surgical procedures that the patients underwent included Roux-en-Y reconstruction (for gastrectomy, gastric bypass, and hepatojejunostomy), PD with Whipple or Child resection, Billroth II gastrectomy and other procedures. The most common indications for sDBE-ERCP were biliary stricture and biliary stones. Table 2 shows the results of the various outcomes of the individual studies.
Table 2
| Author | No. cases | Intact papilla (%) | No. procedures | Enteroscopy success (%) | Diagnostic ERCP success (%) | Therapeutic ERCP success (%) | Overall ERCP success (%) | Complication (%) | Procedure time (min) |
|---|---|---|---|---|---|---|---|---|---|
| Shimatani et al. | 68 | 53 (77.9) | 103 | 100 (97.1) | 98 (98.0) | 98 (100.0) | 98 (95.1) | 5 (4.9) | NA |
| Osoegawa et al. | 28 | 26 (92.9) | 47 | 45 (95.7) | 40 (88.9) | 40 (100.0) | 40 (85.1) | 1 (2.1) | 93.6±6.8 |
| Siddiqui et al. | 79 | 42 (53.2) | 79 | 71 (89.9) | 64 (90.1) | 64 (100.0) | 64 (81.0) | 4 (5.1) | NA |
| Choi et al. | 28 | 28 (100.0) | 32 | 25 (78.1) | 20 (80.0) | 18 (90.0) | 18 (56.3) | 1 (3.1) | 101.2±36.8 |
| Tsutsumi et al. | 72 | 0 (0.0) | 72 | 71 (98.6) | 71 (100.0) | 59 (83.1) | 59 (81.9) | 2 (2.8) | 50 [9–167] |
| Tsou et al. | 47 | 14 (29.8) | 47 | 36 (76.6) | 35 (97.2) | 35 (100.0) | 35 (74.5) | 2 (4.3) | NA |
| Tomoda et al. | 20 | 0 (0.0) | 68 | 65 (95.6) | 62 (95.4) | 62 (100.0) | 62 (91.2) | 2 (2.9) | 75 [42–180] |
| Shimatani et al. | 222 | 97 (46.7) | 280 | 276 (98.6) | 269 (97.5) | 269 (100.0) | 269 (96.1) | 3 (1.1) | 61 [12–252] |
| Yamada et al. | 326 | 111 (34.0) | 326 | 326 (100.0) | 299 (91.7) | 295 (98.7) | 295 (90.5) | 18 (5.5) | NA |
sDBE, short type double balloon enteroscope; ERCP, endoscopic retrograde cholangiopancreatography; NA, not applicable.
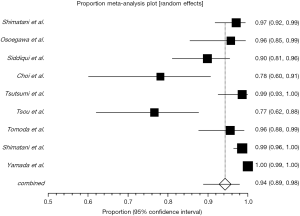
Success of enteroscopy
The enteroscopy success rates among the studies ranged from 76.6% to 100%. The pooled success rate of enteroscopy was 94.3% (95% CI: 88.9–98.0%) (Figure 2). Heterogeneity was significant among the studies (I2=89.3%; P<0.0001). In the only two studies where all patients underwent Roux-en-Y reconstruction the enteroscopy success rate was 76.6% (32) and 78.1% (29), much lower than that in other 7 studies (90–100%) including mixed patients undergoing various surgical procedures other than Roux-en-Y reconstruction (Table 2). In the study by Tsou et al. the enteroscopy success rate was not different between patients undergoing Roux-en-Y reconstruction with intact papilla and with bilioenteric anastomosis, but the mean procedure time was significantly shorter for the former (28 min vs. 52 min, P=0.01) (32). The main causes of failed enteroscopy were severe postsurgical adhesions.
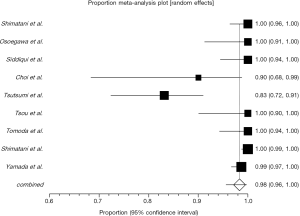
Success of diagnostic ERCP
As shown in Table 2, the success rates of diagnostic ERCP ranged from 80% to 100%. The pooled success rate of diagnostic ERCP was 94.3% (95% CI: 90.8–97.1%) (Figure 3). Heterogeneity was significant among the studies (I2=75.5%; P<0.0001). All patients in the study with the highest success rate of diagnostic ERCP had bilioenteric anastomosis without intact papilla (40). In contrast, the study with the lowest success rate of diagnostic ERCP involved a total of 28 patients who had bariatric Roux-en-Y gastric bypass (RYGB) surgery and intact papilla (29). Diagnostic DBE-ERCP failed because (I) papilla and bilioenteric anastomosis were not identified; (II) bilioenteric anastomosis was totally occluded; (III) it was impossible to advance the wire through severe stricture; and (IV) a periampullary diverticulum was presented.

Success of therapeutic ERCP
The pooled success rate of therapeutic ERCP was 98.3% (95% CI: 95.5–99.7%) (Figure 4). Heterogeneity was significant among the studies (I2=81.9%; P<0.0001). Completed interventions with sDBE-ERCP included sphincterotomy, balloon dilation for pancreaticobiliary duct stricture, pancreaticobiliary stones retrieval, biliary drainage (including endoscopic naso-biliary drainage, plastic and metalic stents), pancreatic drainage (including endoscopic naso-pancreatic drainage and plastic stents), and stent removal.
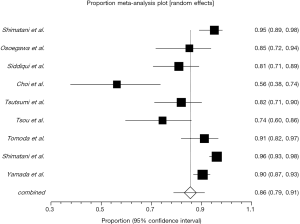
Overall success of sDBE-ERCP
As shown in Table 2, the overall success rates of sDBE-ERCP ranged from 56% to 96%. The pooled overall success rate of ERCP was 85.6% (95% CI: 78.7–91.3%) (Figure 5). Heterogeneity was significant among the studies (I2=86.8%; P<0.0001). The lowest overall success rate of sDBE-ERCP was found in the study involving a total of 28 patients who had bariatric RYGB surgery (29).
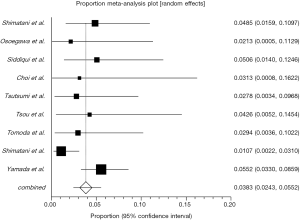
sDBE-ERCP-related complications
sDBE-ERCP-related complications occurred in 38 patients including pancreatitis (n=15), perforation (n=14), cholangitis (n=3), bleeding (n=2), liver graft ischemia (n=1) and 3 adverse events were not reported in details in one study (33). All patients with post-ERCP pancreatitis resolved with conservative treatment without severe acute pancreatitis reported. Among 14 patients with perforation, most of which occurred in pancreaticobiliary limb, 2 patients underwent surgery. The incidence of sDBE-ERCP-related complications was 3.8% (95% CI: 2.4–5.5%) (Figure 6). Heterogeneity was not significant among the studies (I2=33.6%; P=0.1493). There was no death reported in the 9 studies.
Subgroup analysis
The results of the various outcome of ERCP in patients with different reconstructions from eligible studies are presented in Table 3. Subgroup analyses of the endoscopic procedure results in patients with Roux-en-Y reconstruction, patients with PD and patients with Billroth II gastrectomy are shown in Table 4. The enteroscopy success rate (92.1%) and overall success rate (83.8%) in Roux-en-Y group were lower than that in PD (98.7%, 92.2%) and Billroth II gastrectomy (98.6%, 92.9%) group. The diagnostic ERCP success rates of patients in Roux-en-Y (93.5%) and Billroth II gastrectomy group (92.9%) were lower than that of patients in PD group (97.5%).
Table 3
| Different reconstructions | No. procedures | Enteroscopy success (%) | Diagnostic success (%) | Therapeutic success (%) | Overall success (%) |
|---|---|---|---|---|---|
| Patients with Roux-en-Y reconstruction | |||||
| Shimatani et al. | 55 | 52 (94.5) | 50 (96.2) | 50 (100.0) | 50 (90.9) |
| Osoegawa et al. | 25 | 24 (96.0) | 21 (87.5) | 21 (100.0) | 21 (84.0) |
| Siddiqui et al. | 51 | 44 (86.3) | 40 (90.9) | 40 (100.0) | 40 (78.4) |
| Choi et al. | 32 | 25 (78.1) | 20 (80.0) | 18 (90.0) | 18 (56.3) |
| Tsou et al. | 47 | 36 (76.6) | 35 (97.2) | 35 (100.0) | 35 (74.5) |
| Tomoda et al. | 57 | 54 (94.7) | 51 (94.4) | 48 (94.1) | 48 (84.2) |
| Shimatani et al. | 169 | 165 (97.6) | 161 (97.6) | 161 (100.0) | 161 (95.3) |
| Yamada et al. | 220 | 220 (100.0) | 207 (94.1) | 205 (99.0) | 205 (93.2) |
| Patients with PD | |||||
| Shimatani et al. | 26 | 26 (100.0) | 26 (100.0) | 26 (100.0) | 26 (100.0) |
| Osoegawa et al. | 3 | 3 (100.0) | 3 (100) | 3 (100.0) | 3 (100.0) |
| Siddiqui et al. | 20 | 19 (95.0) | 16 (84.2) | 16 (100.0) | 16 (80.0) |
| Tsutsumi et al. | 72 | 71 (98.6) | 71 (100.0) | 59 (83.1) | 59 (81.9) |
| Shimatani et al. | 85 | 85 (100.0) | 84 (98.8) | 84 (100.0) | 84 (98.8) |
| Patients with Billroth II gastrectomy | |||||
| Shimatani et al. | 22 | 22 (100.0) | 22 (100.0) | 22 (100.0) | 22 (100.0) |
| Osoegawa et al. | 18 | 18 (100.0) | 16 (88.9) | 16 (100.0) | 16 (88.9) |
| Siddiqui et al. | 3 | 3 (100.0) | 3 (100.0) | 3 (100.0) | 3 (100.0) |
| Shimatani et al. | 19 | 19 (100.0) | 17 (89.5) | 17 (100.0) | 17 (89.5) |
PD, pancreatoduodenectomy.
Table 4
| Reconstruction type | No. procedures | Enteroscopy success, % (95% CI) | Diagnostic success, % (95% CI) | Therapeutic success, % (95% CI) | Overall success, % (95% CI) |
|---|---|---|---|---|---|
| Roux-en-Y reconstruction | 656 | 92.1 (84.3–97.5) | 93.5 (90.2–96.1) | 98.6 (96.7–99.7) | 83.8 (75.3–90.8) |
| PD | 206 | 98.7 (96.7–99.8) | 97.5 (92.6–99.8) | 96.5 (86.1–100) | 92.2 (79.8–99.0) |
| Billroth II gastrectomy | 62 | 98.6 (94.3–100) | 92.9 (84.0–98.4) | 98.5 (94.0–100) | 92.9 (84.0–98.4) |
PD, pancreatoduodenectomy.
Discussion
This is the first systematic review and meta-analysis to evaluate the efficacy and safety of sDBE-ERCP in the setting of surgically altered anatomy. A total of 890 patients undergoing 1,054 sDBE-ERCP procedures were included in the review. The pooled overall success rate and complication rate were 85.6% and 3.8%, respectively. Our previous meta-analysis on DBE-ERCP, in which most studies were carried out by long DBE, showed a lower overall success rate of 63.55% and a higher complication rate of 6.27% (47). A Japanese multicenter prospective study on sDBE-ERCP showed enteroscopy success rate of 97.7%, diagnostic ERCP success rate of 96.4%, and therapeutic ERCP success rate of 97.9% (48), which were consistent with the results of the present study. It seems that the length of DBE may play a role in the performance of DBE-ERCP in patients with surgically altered anatomy. Our studies indicate that a shorter DBE may benefit ERCP procedure in some patients who underwent gastrointestinal tract reconstructions. The types of gastrointestinal tract reconstruction affect the success rate of the procedure, with overall ERCP success rate of 83.8% in patients with Roux-en-Y reconstruction and Billroth II gastrectomy success being as high as 92.9%.
There are two major challenges to overcome to complete ERCP in patients with surgically altered gastrointestinal anatomy. The first challenge is the deep insertion to find the target sites. In these patients, the anatomical structure of the intestine is substantially altered, and the endoscope needs to be inserted into the pancreaticobiliary limb. The sDBE is of similar construction and features of the conventional long DBE. The sDBE used in all included studies, EC-450BI5/EI-530B (FUJIFILM, Japan), has a 152-cm working length. It entails a mechanism of advancement consisting of sequential bowel pleating by a push-pull technique. The two balloons allow the endoscopist to hold the intestine and to insert the scope deeply while shortening the intestine. This technique enables the scope advancement selectively to reach the blind end in altered gastrointestinal anatomy. The stiff adhesions and sharp angulations of anastomoses may contribute to the failure of enteroscopy. sDBE has better maneuverability than the conventional DBE which allows localization of the pancreaticobiliary limb, visualization of papilla or pancreaticobiliary anastomosis with high success rate. Itoi et al. reported that there was a statistically significant difference in the meantime to reach the papilla between the sDBE and long DBE (29 min vs. 64 min) for patients with Roux-en-Y reconstruction combined with gastrectomy (27). The shorter length of sDBE may be considered disadvantageous in the insertion to a very long blind end. In general, the pooled enteroscopy success rate of this study (94.3%) are not inferior to those obtained using conventional long DBE (3,22-24,26,31,35,38,49). But, the two lowest success rates of enteroscopy (78.1% and 76.6%) were found in studies where all patients had underdone Roux-en-Y reconstructions (29,32). The longer pancreaticobiliary limb in these patients may make it difficult to negotiate the passage of the sDBE to the papilla or pancreaticobiliary anastomosis. The length of the pancreaticobiliary limb is considered to be a determining factor for success of DBE-ERCP and the longest limb is mainly found in patients with RYGB (46). As a result, the sDBE may be too short to reach the blind end in these cases and the conventional DBE may be needed to access to the target sites. Osoegawa et al. found that the mean time to reach the blind end in Billroth II gastrectomy tended to be shorter than that in Roux-en-Y reconstruction (20.9 vs. 37.1 min) during sDBE-ERCP (18). It seems that enteroscopy with sDBE is more difficult in patients with Roux-en-Y reconstruction than that in those with Billroth II gastrectomy. Our subgroup analysis also revealed a lower enteroscopy success rate in Roux-en-Y reconstruction group compared with PD and Billroth II gastrectomy group (Table 4). Therefore, it is important to understand the features and difficulties of each digestive tract reconstruction for successful ERCP with DBE.
The second challenge is the ERCP-related intervention. To complete the DBE-ERCP, it is important not only to insert the scope to the target site but also to successfully cannulate the pancreaticobiliary system. Deep cannulation into biliary/pancreatic duct is an important precondition for next therapeutic procedure. The difficulty of cannulation with DBE is greater than that using a standard duodenoscope because of the long loop of scope, variable position of the target site to the scope end, and lack of an elevator (50). The sDBE may overcome the limitations of the conventional long DBE to result in high success rates for endoscopic intervention. The pooled success rate of diagnostic sDBE-ERCP of this study was 94.3%, which was not inferior to the success rates of cannulation in patients with normal anatomy using standard duodenoscopes (51-53). In a meta-analysis about DEB-ERCP where most studies used conventional long DBE a success rate of diagnostic ERCP of 80% was reported (47). These results demonstrate the good maneuverability of sDBE. The shorter length of sDBE enables the endoscopists to apply pressure more effectively to the enteroscope, which facilitates the cannulation with standard ERCP accessories. By manipulating the scope and the overtube the endoscopist can align the papilla or anastomosis in an axis where the biliary/pancreatic cannulation can be achieved. Various standard sphincterotomes and catheters can be selected to accomplish the cannulation during sDBE-ERCP and, theoretically, would increase the success rate of the selective cannulation in biliary/pancreatic duct. The lowest success rate of diagnostic sDBE-ERCP in this analysis occurred in the study where all patients had intact papilla which appeared in reverse of the usual appearance in normal anatomy (29). Surgically altered anatomy with an intact papilla includes Billroth I/II gastrectomy, subtotal/total gastrectomy with Roux-en-Y anastomosis, and RYGB. The subgroup analysis of the present study showed lower success rate of diagnostic ERCP in Roux-en-Y reconstruction (93.5%) and Billroth II gastrectomy group (92.9%) compared with PD group (97.5%) in which all patients underwent bilioenteric and pancreaticoenteric anastomoses without intact papilla (Table 4). These findings suggest the need of advanced cannulating skills and various endoscopic accessories for the successful cannulation in patients with intact papilla. The balloon fitted to the overtube plays an important role to stabilize the scope and allow the higher maneuverability of the procedure. It has facilitated the operation flow of the cannulation to the biliary/pancreatic duct and the endoscopic treatments more smoothly and safely. Our results showed that once the cannulation is achieved most ERCP-related therapies (98.3%) can be accomplished. In fact, owing to its short length, sDBE allowed endoscopists to carry out any ERCP-related procedures.
In the present study, more than half of the sDBE-ERCP procedures (656/1,054) were performed in patients with Roux-en-Y reconstruction. The overall success rate in patients with Roux-en-Y reconstruction (83.8%) was lower than that in patients with PD (92.2%) and Billroth II gastrectomy (92.9%). Roux-en-Y reconstruction has become the standard technique to drain the pancreaticobiliary system for patients who undergo gastrointestinal or pancreaticobiliary surgeries (54). After Roux-en-Y reconstruction, some patients are predisposed to pancreaticobiliary disorders which may need endoscopic interventions (29,55). ERCP in patients with a Roux-en-Y reconstruction are challenging using standard side-viewing duodenoscope or enteroscope with success rates of 33–67% (4,11,12,56,57). Investigation of the factor contributing to the failed DBE-ERCP by multivariate analysis revealed that Roux-en-Y reconstruction was associated with DBE-ERCP failure (58). In Roux-en-Y reconstruction, there are cases with or without gastrectomy. In cases with gastrectomy, there are partial gastrectomy and total gastrectomy. These differences affect the difficulty of scope insertion. Tomoda et al. found that cases with total gastrectomy are easier to perform the scope insertion in comparison with cases without gastrectomy (59). A study revealed that the time needed to get blind end in patients without gastrectomy was longer than that in patients with gastrectomy (52 min vs. 28 min) (32). The intact stomach predisposed the enteroscope to loop along greater curvature, making the maneuverability more difficult and resulting in a prolonged procedure time. It is felt that the two major components determining ERCP success were the length of Roux limb and whether the patient had an intact papilla or anastomosis (25,27,28). The length of Roux limb varies greatly depending on the indication for Roux-en-Y reconstruction. ERCP through shorter nonbariatric Roux limbs can often be accomplished with pediatric or adult colonoscopes, or even a duodenoscope in rare cases. The longest Roux limbs are usually found in patients with bariatric RYGB and this total length from mouth to the papilla may exceed 300 cm (60-62), well beyond the access of sDBE. Long or very long limb (>150 cm) reconstructions are often performed in revisional bariatric operations in patients with inadequate weight loss. As a result, the sDBE became too short to reach the blind end (28). Some endoscopists even considered RYGB as the most difficult type of reconstruction in which to successfully reach the blind end with sDBE (46). In such cases a long DBE may be needed to complete the procedure. With respect to the cannulation of sDBE-ERCP, patients with Roux-en-Y reconstruction can be divided into two groups: with intact papilla and bilioenteric anastomosis. The two groups of patients present different difficulty in cannulation of sDBE-ERCP. It is believed that cannulating an intact papilla is much more difficult than a bilioenteric anastomosis (26,27). A study did show that the mean time of cannulation of sDBE-ERCP in group with intact papilla was longer than that in group with bilioenteric anastomosis (28.4 vs. 4 min, P<0.001) (32). The sDBE is a forward-viewing instrument, which provides suboptimal viewing angles when performing ERCP in an intact papilla. Some techniques are helpful to increase the cannulation success rate in patients with intact papilla, including locating the papilla in a 6 o’clock direction, using straight catheter, and adopting vacuuming force and down-angling maneuver. In combination of with these techniques, the axis of the biliary duct may be aligned with the axis of the catheter, which facilities the deep cannulation (63). Among all bariatric operations, RYGB is considered the gold standard (64). RYGB accounts for more than 60% of bariatric procedures performed in the United States (61,65). With the obesity epidemic and the high prevalence of obesity related comorbidities (66), endoscopists will encounter more patients with pancreaticobiliary diseases who had undergone RYGB in the future.
ERCP in patients with surgically altered anatomy may be associated with both usual and additional risks compared with standard ERCP. Complications of DBE-ERCP-related procedures for surgically altered anatomy mainly include perforation, bleeding, cholangitis, and pancreatitis. A higher incidence of complications was observed in patients with surgically altered anatomy who underwent ERCP compared with patients with normal anatomy (67,68). The rate of complications of ERCP assisted with small bowel enteroscopies range from 0–19% (69). The complication rate of ERCP in patients with Roux-en-Y reconstruction has been reported to be 5% (27). For a more meaningful analysis, we excluded reports with less than 10 cases with the intent to limit the potential negative effect of the learning curve of the procedure, i.e., a possible overestimation of the complication rate. The most common complication in the present study is pancreatitis. In patients with bilioenteric anastomosis the risk of post-ERCP pancreatitis is negligible, but the sDBE procedure may induce pancreatitis even without intervention in papilla or pancreatic duct. So, the patients should be closely observed after the procedure to rule out pancreatitis. The second common complication of the current study is perforation which is considered the most severe complication of DBE-ERCP. Although most cases improved with conservative management, some required surgical operation. Barotrauma is the major cause of intestinal perforation and may be a result of excessive air insufflation forming a close loop between the blind end and the inflated overtube or enteroscope balloon (70). Use of carbon dioxide insufflations instead of air insufflations may reduce this risk. Patients requiring nonemergent ERCP soon after surgery should wait at least 2 weeks to allow the anastomoses to heal properly and avoid disrupting sutures and reconstructions. Our previous study reported a complication rate of 6.27% of DBE-ERCP in patients with surgically altered anatomy (47) and the incidence of complication of 3.8% in the present study may imply a better safety of sDBE-ERCP. Such procedures appear to have an acceptable safety profile.
There are some limitations in our analysis. All studies included are retrospective studies with innate bias. The studies included in the analysis were heterogenic, mainly because there were obvious varieties among patients in term of underlying diseases and indications for ERCP. A study used some techniques during sDBE-ERCP, such as attachment hood or CO2 insufflation (18), which were not adopted in other studies.
Conclusions
In conclusion, sDBE-ERCP is an effective and safe modality for patients with pancreaticobiliary diseases who have undergone bowel reconstruction. The main advantage of sDBE-ERCP is the use of commercially available ERCP accessories compared with the conventional DBE because of the shorter length of sDBE. For patients with longer pancreaticobiliary limb, especially RYGB, it is reasonable to attempt sDBE-ERCP first and use a long DBE as a rescue tool in case sDBE cannot reach the target site. There are controversies about which balloon assisted enteroscope is most suitable for this procedure. To answer the question, further randomized controlled trials for the same gastrointestinal tract reconstructions are warranted.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2019.09.04). Dr. Qi serves as an Editor-in-Chief of AME Medical Journal. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cotton PB. Fifty years of ERCP: A personal review. Gastrointest Endosc 2018;88:393-6. [Crossref] [PubMed]
- Freeman ML, Guda NM. ERCP cannulation: A review of reported techniques. Gastrointest Endosc 2005;61:112-25. [Crossref] [PubMed]
- Mönkemüller K, Fry LC, Bellutti M, et al. ERCP with the double balloon enteroscope in patients with Roux-en-Y anastomosis. Surg Endosc 2009;23:1961-7. [Crossref] [PubMed]
- Chahal P, Baron TH, Topazian MD, et al. Endoscopic retrograde cholangiopancreatography in post-Whipple patients. Endoscopy 2006;38:1241-5. [Crossref] [PubMed]
- Forbes A, Cotton PB. ERCP and sphincterotomy after Billroth II gastrectomy. Gut 1984;25:971-4. [Crossref] [PubMed]
- Kim MH, Lee SK, Lee MH, et al. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: A comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy 1997;29:82-5. [Crossref] [PubMed]
- Aabakken L, Holthe B, Sandstad O, et al. Endoscopic pancreaticobiliary procedures in patients with a Billroth II resection: A 10-year follow-up study. Ital J Gastroenterol Hepatol 1998;30:301-5. [PubMed]
- Bergman JJ, van Berkel AM, Bruno MJ, et al. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc 2001;53:19-26. [Crossref] [PubMed]
- Lin LF, Siauw CP, Ho KS, et al. ERCP in post-Billroth II gastrectomy patients: emphasis on technique. Am J Gastroenterol 1999;94:144-8. [Crossref] [PubMed]
- Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut 1986;27:1193-8. [Crossref] [PubMed]
- Hintze RE, Adler A, Veltzke W, et al. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with billroth II or Roux-en-Y gastrojejunostomy. Endoscopy 1997;29:69-73. [Crossref] [PubMed]
- Wright BE, Cass OW, Freeman ML. ERCP in patients with long-limb Roux-en-Y gastrojejunostomy and intact papilla. Gastrointest Endosc 2002;56:225-32. [Crossref] [PubMed]
- Teplick SK, Flick P, Brandon JC. Transhepatic cholangiography in patients with suspected biliary disease and nondilated intrahepatic bile ducts. Gastrointest Radiol 1991;16:193-7. [Crossref] [PubMed]
- Fontein DB, Gibson RN, Collier NA, et al. Two decades of percutaneous transjejunal biliary intervention for benign biliary disease: A review of the intervention nature and complications. Insights Imaging 2011;2:557-65. [Crossref] [PubMed]
- Yamamoto H, Sekine Y, Sato Y, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc 2001;53:216-20. [Crossref] [PubMed]
- Yamamoto H. Fifteen Years Since the Advent of Double-Balloon Endoscopy. Clin Gastroenterol Hepatol 2017;15:1647-50. [Crossref] [PubMed]
- Itoi T, Ishii K, Sofuni A, et al. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol 2010;105:93-99. [Crossref] [PubMed]
- Osoegawa T, Motomura Y, Akahoshi K, et al. Improved techniques for double-balloon-enteroscopy-assisted endoscopic retrograde cholangiopancreatography. World J Gastroenterol 2012;18:6843-9. [Crossref] [PubMed]
- Haber GB. Double balloon endoscopy for pancreatic and biliary access in altered anatomy (with videos). Gastrointest Endosc 2007;66:S47-50. [Crossref] [PubMed]
- Chu YC, Su SJ, Yang CC. Gastrointest Endosc 2007;66:1234-6. [Crossref] [PubMed]
- Haruta H, Yamamoto H, Mizuta K, et al. A case of successful enteroscopic balloon dilation for late anastomotic stricture of choledochojejunostomy after living donor liver transplantation. Liver Transpl 2005;11:1608-10. [Crossref] [PubMed]
- Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: A case series. Gastrointest Endosc 2007;66:1038-41. [Crossref] [PubMed]
- Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy 2007;39:1068-71. [Crossref] [PubMed]
- Pohl J, May A, Aschmoneit I, et al. Double-balloon endoscopy for retrograde cholangiography in patients with choledochojejunostomy and Roux-en-Y reconstruction. Z Gastroenterol 2009;47:215-9. [Crossref] [PubMed]
- Shimatani M, Matsushita M, Takaoka M, et al. Effective "short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: A large case series. Endoscopy 2009;41:849-54. [Crossref] [PubMed]
- Parlak E, Ciçek B, Dişibeyaz S, et al. Endoscopic retrograde cholangiography by double balloon enteroscopy in patients with Roux-en-Y hepaticojejunostomy. Surg Endosc 2010;24:466-70. [Crossref] [PubMed]
- Itoi T, Ishii K, Sofuni A, et al. Long- and short-type double-balloon enteroscopy-assisted therapeutic ERCP for intact papilla in patients with a Roux-en-Y anastomosis. Surg Endosc 2011;25:713-21. [Crossref] [PubMed]
- Siddiqui AA, Chaaya A, Shelton C, et al. Utility of the short double-balloon enteroscope to perform pancreaticobiliary interventions in patients with surgically altered anatomy in a US multicenter study. Dig Dis Sci 2013;58:858-64. [Crossref] [PubMed]
- Choi EK, Chiorean MV, Coté GA, et al. ERCP via gastrostomy vs. double balloon enteroscopy in patients with prior bariatric Roux-en-Y gastric bypass surgery. Surg Endosc 2013;27:2894-9. [Crossref] [PubMed]
- Ryozawa S, Iwamoto S, Iwano H, et al. ERCP using double-balloon endoscopes in patients with Roux-en-Y anastomosis. J Hepatobiliary Pancreat Surg 2009;16:613-7. [Crossref] [PubMed]
- Raithel M, Dormann H, Naegel A, et al. Double-balloon-enteroscopy-based endoscopic retrograde cholangiopancreatography in post-surgical patients. World J Gastroenterol 2011;17:2302-14. [Crossref] [PubMed]
- Tsou YK, Lee MS, Chen KF, et al. Double-balloon enteroscopy-assisted endoscopic retrograde cholangiography for Roux-en-Y reconstruction patients with papilla of Vater or bilioenteric anastomosis. Scand J Gastroenterol 2016;51:95-102. [Crossref] [PubMed]
- Shimatani M, Tokuhara M, Masuda M, et al. Utility of newly developed short type double balloon endoscopy for ERCP in postoperative patients with surgical anatomic variations; a large case series. United Eur Gastroent 2017;5:A44-A45.
- Shah RJ, Smolkin M, Yen R, et al. A multicenter, U. S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc 2013;77:593-600. [Crossref] [PubMed]
- Mönkemüller K, Bellutti M, Neumann H, et al. Therapeutic ERCP with the double-balloon enteroscope in patients with Roux-en-Y anastomosis. Gastrointest Endosc 2008;67:992-6. [Crossref] [PubMed]
- Shimatani M, Takaoka M, Ikeura T, et al. Evaluation of endoscopic retrograde cholangiopancreatography using a newly developed short-type single-balloon endoscope in patients with altered gastrointestinal anatomy. Dig Endosc 2014;26:147-55. [Crossref] [PubMed]
- Matsushita M, Shimatani M, Takaoka M, et al. "Short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy. Am J Gastroenterol 2008;103:3218-9. [Crossref] [PubMed]
- Chu YC, Yang CC, Yeh YH, et al. Double-balloon enteroscopy application in biliary tract disease-its therapeutic and diagnostic functions. Gastrointest Endosc 2008;68:585-91. [Crossref] [PubMed]
- Tsujino T, Yamada A, Isayama H, et al. Experiences of biliary interventions using short double-balloon enteroscopy in patients with Roux-en-Y anastomosis or hepaticojejunostomy. Dig Endosc 2010;22:211-6. [Crossref] [PubMed]
- Tsutsumi K, Kato H, Muro S, et al. ERCP using a short double-balloon enteroscope in patients with prior pancreatoduodenectomy: higher maneuverability supplied by the efferent-limb route. Surg Endosc 2015;29:1944-51. [Crossref] [PubMed]
- Liu K, Joshi V, Saxena P, et al. Predictors of success for double balloon-assisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y anastomosis. Dig Endosc 2017;29:190-7. [Crossref] [PubMed]
- Tomoda T, Tsutsumi K, Kato H, et al. Outcomes of management for biliary stricture after living donor liver transplantation with hepaticojejunostomy using short-type double-balloon enteroscopy. Surg Endosc 2016;30:5338-44. [Crossref] [PubMed]
- Yamada A, Kogure H, Nakai Y, et al. Performance of a new short-type double-balloon endoscope with advanced force transmission and adaptive bending for pancreaticobiliary intervention in patients with surgically altered anatomy: A propensity-matched analysis. Dig Endosc 2019;31:86-93. [Crossref] [PubMed]
- Cheung SW, Cheng KS, Yip WM, et al. Feasibility of short double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered gastrointestinal anatomy: experience in a regional centre. Hong Kong Med J 2017;23:648-50. [Crossref] [PubMed]
- Tsutsumi K, Kato H, Okada H. Impact of a Newly Developed Short Double-Balloon Enteroscope on Stent Placement in Patients with Surgically Altered Anatomies. Gut and Liver 2017;11:306-11. [Crossref] [PubMed]
- Kato H, Tsutsumi K, Harada R, et al. Short double-balloon enteroscopy is feasible and effective for endoscopic retrograde cholangiopancreatography in patients with surgically altered gastrointestinal anatomy. Digestive Endoscopy 2014;26:130-5. [Crossref] [PubMed]
- Shao XD, Qi XS, Guo XZ. Endoscopic retrograde cholangiopancreatography with double balloon enteroscope in patients with altered gastrointestinal anatomy: A meta-analysis. Saudi J Gastroenterol 2017;23:150-60. [PubMed]
- Shimatani M, Hatanaka H, Kogure H, et al. Diagnostic and Therapeutic Endoscopic Retrograde Cholangiography Using a Short-Type Double-Balloon Endoscope in Patients With Altered Gastrointestinal Anatomy: A Multicenter Prospective Study in Japan. Am J Gastroenterol 2016;111:1750-8. [Crossref] [PubMed]
- Maaser C, Lenze F, Bokemeyer M, et al. Double balloon enteroscopy: A useful tool for diagnostic and therapeutic procedures in the pancreaticobiliary system. Am J Gastroenterol 2008;103:894-900. [Crossref] [PubMed]
- Ito K, Masu K, Kanno Y, et al. Ampullary intervention for bile duct stones in patients with surgically altered anatomy. Digestive Endoscopy 2014;26:116-21. [Crossref] [PubMed]
- Bailey AA, Bourke MJ, Williams SJ, et al. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy 2008;40:296-301. [Crossref] [PubMed]
- Cheung J, Tsoi KK, Quan WL, et al. Guidewire versus conventional contrast cannulation of the common bile duct for the prevention of post-ERCP pancreatitis: A systematic review and meta-analysis. Gastrointest Endosc 2009;70:1211-9. [Crossref] [PubMed]
- Tse F, Yuan Y, Moayyedi P, et al. Guide wire-assisted cannulation for the prevention of post-ERCP pancreatitis: A systematic review and meta-analysis. Endoscopy 2013;45:605-18. [Crossref] [PubMed]
- Moreels TG. Altered anatomy: enteroscopy and ERCP procedure. Best Pract Res Clin Gastroenterol 2012;26:347-57. [Crossref] [PubMed]
- Saidi RF, Elias N, Ko DS, et al. Biliary reconstruction and complications after living-donor liver transplantation. HPB 2009;11:505-9. [Crossref] [PubMed]
- Feitoza AB, Baron TH. Endoscopy and ERCP in the setting of previous upper GI tract surgery. Part II: postsurgical anatomy with alteration of the pancreaticobiliary tree. Gastrointest Endosc 2002;55:75-9. [Crossref] [PubMed]
- Elton E, Hanson BL, Qaseem T, et al. Diagnostic and therapeutic ERCP using an enteroscope and a pediatric colonoscope in long-limb surgical bypass patients. Gastrointest Endosc 1998;47:62-7. [Crossref] [PubMed]
- Sakakihara I, Kato H, Muro S, et al. Double-balloon enteroscopy for choledochojejunal anastomotic stenosis after hepato-biliary-pancreatic operation. Dig Endosc 2015;27:146-54. [Crossref] [PubMed]
- Tomoda T, Tsutsumi K, Okada H. Comparison between Roux-en-Y patients with and without gastrectomy during endoscopic retrograde cholangiopancreatography using a short double-balloon enteroscope. Dig Endosc 2015;27:775. [Crossref] [PubMed]
- Ross AS. Endoscopic retrograde cholangiopancreatography in the surgically modified gastrointestinal tract. Gastrointest Endosc Clin N Am 2009;19:497-507. [Crossref] [PubMed]
- Khashab MA, Okolo PI 3rd. Accessing the pancreatobiliary limb and ERCP in the bariatric patient. Gastrointest Endosc Clin N Am 2011;21:305-13. [Crossref] [PubMed]
- Lopes TL, Wilcox CM. Endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y anatomy. Gastroenterol Clin North Am 2010;39:99-107. [Crossref] [PubMed]
- Shimatani M, Takaoka M, Okazaki K. Tips for double balloon enteroscopy in patients with Roux-en-Y reconstruction and modified child surgery. J Hepatobiliary Pancreat Sci 2014;21:E22-8. [Crossref] [PubMed]
- Needleman BJ, Happel LC. Bariatric surgery: choosing the optimal procedure. Surg Clin North Am 2008;88:991-1007. [Crossref] [PubMed]
- Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA 2005;294:1909-17. [Crossref] [PubMed]
- Nguyen DM, El-Serag HB. The big burden of obesity. Gastrointest Endosc 2009;70:752-7. [Crossref] [PubMed]
- Bagci S, Tuzun A, Ates Y, et al. Efficacy and safety of endoscopic retrograde cholangiopancreatography in patients with Billroth II anastomosis. Hepatogastroenterology 2005;52:356-9. [PubMed]
- Faylona JM, Qadir A, Chan AC, et al. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy 1999;31:546-9. [Crossref] [PubMed]
- Moreels TG. Endoscopic retrograde cholangiopancreatography in patients with altered anatomy: How to deal with the challenges? World J Gastrointest Endosc 2014;6:345-51. [Crossref] [PubMed]
- De Koning M, Moreels TG. Comparison of double-balloon and single-balloon enteroscope for therapeutic endoscopic retrograde cholangiography after Roux-en-Y small bowel surgery. BMC Gastroenterol 2016;16:98. [Crossref] [PubMed]
Cite this article as: Shao XD, Qi XS, Wang R, Guo XZ. Performance of short type double balloon enteroscope in endoscopic retrograde cholangiopancreatography: does the length of a scope matter?—a systematic review and meta-analysis. AME Med J 2019;4:38.

