
Extrarenal adult Wilms’ tumor case report
Introduction
Although Wilms’ tumors (WTs) is the most common renal malignancy in childhood, presentation in adults is very rare (1-4). Extrarenal presentation of WTs is also an unusual presentation, with studies often limited to case reports (5,6). Due to the rarity of extrarenal adult WTs, treatment guidelines are limited (7). Current guidelines for extrarenal adult WTs suggest similar treatment regimes as childhood and renal WTs; however, various studies question the effectiveness of these guidelines as external adult WTs are an abnormal and rare variant of WTs (1,5). We report a case of adult extrarenal WT, and review the literature on management. We present the following case in accordance with the CARE Guideline.
Case presentation
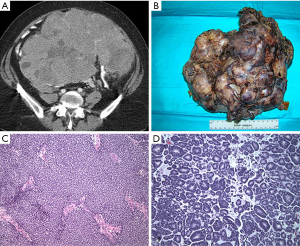
A 50-year-old female presented with abdominal discomfort and distention. An abdominal/pelvic CT revealed a 30 cm abdominal mass (Figures 1,2). A percutaneous biopsy was consistent with Wilms’ tumor, which is extremely rare in adult patients and in extrarenal location. Neoadjuvant dactinomycin based chemotherapy resulted in a 30% regression in tumor size. Subsequent surgical resection was successful in removing this over 20 cm (7.3 lb) Wilms tumor, with negative surgical margins (Figure 3). Gross pathology showed the typical solid and tan appearance, with evidence of cystic changes (Figure 1B). On microscopy, a combination of stroma and blastema cells, with epithelial component forming tubules was noted (Figure 1C,D). Despite proceeding with adjuvant chemotherapy, the patient recurred and succumbed to disease.
Discussion
Wilm’s tumor (WT) is the most common primary renal malignancy in children (1-3). Management follows risk stratified protocols set out by the National Wilms’ Tumour Study Group (NWTS) in North America and the Society of Paediatric Oncology (SIOP) in Europe. The NWTS prefers a surgery first approach, with subsequent adjuvant chemotherapy and radiotherapy based on surgical staging. Conversely the SIOP approach is to give neoadjuvant chemotherapy to all comers, followed by surgical resection, and then adjuvant therapies based on staging. Both groups have demonstrated excellent survival outcomes with protocol driven treatment for pediatric WT.
In adults, WT is extremely rare. Reported incidence is 0.2 per million per year and this comprises 3% of all WT cases (4,8). Extrarenal adult WT is even rarer, with only a small number of reported cases in the literature. These have included tumors arising from the uterus, ovary, testis, and retroperitoneum (6,9-13). Although evidence is limited by scarcity of reports, it is felt to behave in a similar fashion to classic WT, and should be treated with the same therapeutic approach (5).
The clinical presentation of WT in adults is distinct from that in children. While children often present asymptomatically, with an enlarging abdominal mass, adults frequently present with flank pain, weight loss, and decreased performance status (2). Histologically, pediatric and adult WT are identical, characterized by the presence of epithelial, stromal, and blastemal elements (14). The diagnosis of adult WT is based on fulfilling the Kilton criteria. These are: (I) primary renal neoplasm, (II) primitive blastematous spindle or round cell component, (III) formation of abortive or embryonal tubular or glomeruloid structures, (IV) no area of tumor diagnostic of renal cell carcinoma, (V) confirmation of histology and (VI) age >15 years (15).
Despite their shared histology, adult WT are traditionally thought to portend a significantly worse prognosis than pediatric WT. The reasons for this are multifactorial. Adult patients tend to present with more advance stages of disease, including higher frequency of metastases (1,2,7,8,14,16). In addition, WT in adults represents a diagnostic dilemma, as the clinical and radiographic features are indistinguishable from more common adult renal neoplasms such as renal cell carcinoma (16). Pretreatment biopsy can assist in making the diagnosis, but is not routinely used in all centers. In our case, it allowed us to diagnose the WT and deliver neoadjuvant chemotherapy, prior to proceeding with surgery.
Further, given its rarity, there is a lack of familiarity with WT amongst adult pathologists and oncologists, which combined with diagnostic dilemma, puts patients are at risk of under treatment from non-compliance with the recommended pediatric protocols (1,17). Finally, even when receiving treatment as per the standard of care protocols, adults tend to experience worse toxicity from the chemotherapy, which can limit treatment (18-20). Notwithstanding these challenges, both the NWTS and the SIOP groups have demonstrated improved outcomes for adult patients with WT through the strict application of the pediatric protocols.
Kalapurakal et al. reviewed 23 adults with favorable histology Wilms tumour. Ten patients (43%) had advanced disease (stage III & IV) (16). All tumors underwent centralized pathology review to confirm the diagnosis. All patients were treated with primary nephrectomy followed by adjuvant chemotherapy and in some cases radiotherapy, as per the pediatric NWTS protocols. The 5-year overall survival was 83% and they recommended that therapy in adults with favorable histology WT should be directed according to pediatric NWTS protocols.
Reihard et al. reviewed 30 adults with WT treated as per the pediatric SIOP protocols. Of note, 10 patients (33%) had metastases on presentation (2). In this series, the majority of patients started with nephrectomy, although some did first undergo biopsy and neoadjuvant chemotherapy. All patients received adjuvant chemotherapy as per the SIOP risk stratified protocols, and adjuvant radiotherapy was delivered in 46.7% of cases. With a median FU of 4 years, overall survival was 83%, similar to the NWTS results. The authors concluded that adults can be cured in a high percentage by a multimodal treatment according to pediatric protocols.
In summary, we present a case of extrarenal Wilms’ tumor in an adult female patient. She underwent percutaneous biopsy of a retroperitoneal mass confirming WT. This was followed by neoadjuvant chemotherapy, complete surgical resection with negative margins, and finally further adjuvant chemotherapy. Despite this, the patient succumbed to the disease. Adult WT is a rare entity which presents with flank pain, weight loss, and decreased performance status. Treatment should follow the established protocols (NWTS or SIOP) for pediatric WT in order to maximize overall survival. With strict protocol adherence, good outcomes can be achieved, even in advanced disease states.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Philippe E. Spiess) for the series “Rare Genitourinary Malignancies” published in AME Medical Journal. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2019.11.01). The series “Rare Genitourinary Malignancies” was commissioned by the editorial office without any funding or sponsorship. Dr. Spiess served as the unpaid Guest Editor of the series and serves as an unpaid Associate Editor-in-Chief of AME Medical Journal from Sep 2017 to Feb 2020. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Terenziani M, Spreafico F, Collini P, et al. Adult Wilms' tumor: A monoinstitutional experience and a review of the literature. Cancer 2004;101:289-93. [Crossref] [PubMed]
- Reinhard H, Aliani S, Ruebe C, et al. Wilms' tumor in adults: results of the Society of Pediatric Oncology (SIOP) 93-01/Society for Pediatric Oncology and Hematology (GPOH) Study. J Clin Oncol 2004;22:4500-6. [Crossref] [PubMed]
- Arrigo S, Beckwith JB, Sharples K, et al. Better survival after combined modality care for adults with Wilms' tumor. A report from the National Wilms' Tumor Study. Cancer 1990;66:827-30. [Crossref] [PubMed]
- Mitry E, Ciccolallo L, Coleman MP, et al. Incidence of and survival from Wilms' tumour in adults in Europe: data from the EUROCARE study. Eur J Cancer 2006;42:2363-8. [Crossref] [PubMed]
- Coppes MJ, Wilson PC, Weitzman S. Extrarenal Wilms' tumor: staging, treatment, and prognosis. J Clin Oncol 1991;9:167-74. [Crossref] [PubMed]
- Koretz MJ, Wang S, Klein FA, et al. Extrarenal adult Wilms' tumor. Cancer 1987;60:2484-8. [Crossref] [PubMed]
- Orditura M, De Vita F, Catalano G. Adult Wilms' tumor: a case report. Cancer 1997;80:1961-5. [Crossref] [PubMed]
- Bozeman G, Bissada NK, Abboud MR, et al. Adult Wilms' tumor: prognostic and management considerations. Urology 1995;45:1055-8. [Crossref] [PubMed]
- Muc RS, Grayson W, Grobbelaar JJ. Adult extrarenal Wilms tumor occurring in the uterus. Arch Pathol Lab Med 2001;125:1081-3. [PubMed]
- Isaac MA, Vijayalakshmi S, Madhu CS, et al. Pure cystic nephroblastoma of the ovary with a review of extrarenal Wilms' tumors. Hum Pathol 2000;31:761-4. [Crossref] [PubMed]
- Fukutomi Y, Shibuya C, Yamamoto S, et al. Extrarenal Wilms' tumor in the adult patient. A case report and review of the world literature. Am J Clin Pathol 1988;90:618-22. [Crossref] [PubMed]
- Gillis AJ, Oosterhuis JW, Schipper ME, et al. Origin and biology of a testicular Wilms' tumor. Genes Chromosomes Cancer 1994;11:126-35. [Crossref] [PubMed]
- Kadota K, Haba R, Kushida Y, et al. Adult extrarenal Wilms' tumor mimicking mixed epithelial and stromal tumor in the retroperitoneum: a case report with immunohistochemical study and review of the literature. Pathol Oncol Res 2009;15:665-9. [Crossref] [PubMed]
- Huszno J, Starzyczny-Słota D, Jaworska M, et al. Adult Wilms' tumor - diagnosis and current therapy. Cent European J Urol 2013;66:39-44. [Crossref] [PubMed]
- Kilton L, Matthews MJ, Cohen MH. Adult Wilms tumor: a report of prolonged survival and review of literature. J Urol 1980;124:1-5. [Crossref] [PubMed]
- Kalapurakal JA, Nan B, Norkool P, et al. Treatment outcomes in adults with favorable histologic type Wilms tumor-an update from the National Wilms Tumor Study Group. Int J Radiat Oncol Biol Phys 2004;60:1379-84. [Crossref] [PubMed]
- Segers H. Management of adults with Wilms' tumor: recommendations based on international consensus. Expert Rev Anticancer Ther 2011;11:1105-13. [Crossref] [PubMed]
- Ali EM, Elnashar AT. Adult Wilms' tumor: review of literature. J Oncol Pharm Pract 2012;18:148-51. [Crossref] [PubMed]
- Geethamani V, Kusuma V, Gowda KMS, et al. Adult Wilms' tumour: a case report with review of literature. Diagn Pathol 2006;1:46. [Crossref] [PubMed]
- Kumar A, Lal B, Singh M, et al. Adult Wilms' tumor: report of a case and review of the literature. Jpn J Surg 1990;20:585-9. [Crossref] [PubMed]
Cite this article as: Beech BB, Carlock HR, Rudzinski JK, Martinez DR, Dhillon J, Spiess PE. Extrarenal adult Wilms’ tumor case report. AME Med J 2019;4:40.



