Off-pump coronary artery bypass grafting
Introduction
In the current era of substantial increase in coronary angioplasty volumes and concomitant reduction in surgical myocardial revascularization rates, coronary artery bypass grafting (CABG) is still regarded as the benchmark treatment for three-vessel coronary artery disease or left main stem stenosis (1). Surgical myocardial revascularization performed with the assistance of cardiopulmonary bypass (CPB) and cardioplegic arrest, commonly known as conventional or on-pump CABG, is considered the gold standard (2). However, numerous physiologic disturbances affecting the hemostatic mechanisms, immune mediators and inflammatory responses are sequelae of CABG on CPB that culminate in deterioration of function of various organs. Furthermore, handling of an atherosclerotic ascending aorta during cannulation and cross-clamping can enhance embolization and stroke risk (2). Appreciation of these deleterious effects of on-pump CABG prompted revival of off-pump CABG nearly quarter of a century ago (3).
Off-pump CABG since its renaissance has been intensely scrutinized and attracted negative criticism. Whereas a large number of retrospective nonrandomized observational studies, prospective randomized controlled trials (RCTs), and meta-analyses have verified the status of off-pump CABG as a safe and effective technique (4), the larger and more modern randomized trials have been unable to demonstrate absolute supremacy of off-pump CABG over on-pump CABG (5-8). In fact, concerns about completeness of revascularization, suboptimal graft patency and long-term survival have prevented it from being adopted worldwide (8,9). This review describes the evolution, indications, contraindications, technique, and outcomes of off-pump CABG as well as concerns and controversies ascribed to it.
Evolution
Off-pump CABG is frequently considered a modern technique; however, archives of surgical myocardial revascularization reveal that several revolutionary revascularization procedures were conducted off-pump without the assistance of CPB (Table 1). Vineberg procedure involving direct insertion of the left internal mammary artery (LIMA) into the ischemic myocardium was performed without the support of heart lung machine (10). Bailey in 1957 (11) and Longmire a year later (12) described techniques of coronary endarterectomy undertaken without the aid of CPB. Although Favaloro, in 1968, brought into vogue on-pump CABG using long saphenous vein as the conduit for grafting (13), Kolessov had already performed off-pump CABG using LIMA, in 1967 (14). In 1975, Trapp (15) and also Ankeney (16) published their pioneering work of beating heart revascularization of the right and left anterior descending (LAD) coronary arteries. The publication of these landmark reports coincided with standardization of the safety of perfusion techniques and development of methods to protect the myocardium by using cold cardioplegia. The technical benefits of operating on an arrested, flaccid heart in a bloodless field far outweighed the risk of myocardial damage, subsequent to transient disruption of coronary blood flow during off-pump CABG, resulting in abandonment of this technique by most surgeons (17).
Table 1
| Year | Development |
|---|---|
| 1876 | Adam Hammer establishes the pathophysiology of coronary artery disease |
| 1910 | Alexis Carrel first describes CABG in animals |
| 1950 | Vineberg first to implant internal mammary artery into the myocardium |
| 1953 | Gordon Murray reported experimental placement of arterial grafts into the coronary circulation |
| 1955 | Sidney Smith first to harvest long saphenous vein and use it as an aorto-coronary conduit |
| 1957 | Bailey reports first successful coronary endarterectomy in man on beating heart |
| 1958 | Longmire reports another open coronary endarterectomy without CPB |
| 1960 | Goetz et al. reported non-suture method using tantalum rings for coronary anastomosis |
| 1964 | Kolesov performs successful internal mammary artery to coronary artery anastomosis in humans on the beating heart |
| 1967 | Favaloro performs successful CABG in humans using saphenous veins |
| 1990s | Benetti, Calafiore, Subramanian achieve direct anastomoses between LIMA and LAD artery on beating hearts, operating through 10 cm incision between ribs |
| 1995 | Launch of products to enable beating heart multivessel CABG through median sternotomy |
| 1997 | Octopus®, the first tissue suction stabilizer for beating heart CABG launched |
| 1998 | Duhaylongsod, Mayfield and Wolf report successful thoracoscopic harvesting of LIMA at various centers |
| 2000 | Falk, Diegeler, Walther, Auschbach and Mohr report a succession of developments in minimally invasive robotic surgery |
CABG, coronary artery bypass grafting; CPB, cardiopulmonary bypass; LIMA, left internal mammary artery; LAD, left anterior descending. Reprinted with permission from Springer Nature Customer Service Centre GmbH: Raja SG. editor. Cardiac Surgery: A Complete Guide. Springer Nature, Copyright 2020. doi: https://doi.org/10.1007/978-3-030-24174-2.
In 1990s, the interest in performing off-pump CABG was reinvigorated (18). This resurgence was the result of recognition of the damaging effects of CPB as well as development of devices and strategies to perform beating heart bypass surgery safely. In 2002 off-pump CABG was at its zenith in the United States with almost 23% of CABG procedures performed without pump and this popularity dwindled to 17% by 2012 (19). The adoption rates globally show a large variation and are impacted by availability of novel devices, innovative strategies and emerging publications.
Indications
Major advances in procedural performance and development of innovative devices have enabled beating heart bypass surgery to being offered to an increasing number of patients. Currently off-pump CABG is indicated on its own for treatment of single as well as multivessel coronary artery disease and can be combined with coronary angioplasty (18) and transcatheter aortic valve implantation (20) as a hybrid procedure. Patients with impaired left ventricular function, left mainstem stenosis, advanced age, cerebrovascular accidents, chronic renal failure, chronic obstructive pulmonary disease, sleep apnea syndrome, atheromatous disease of the aorta, acute myocardial infarction (MI), and reoperations are all candidates for off-pump CABG (18). Off-pump CABG has also been done in combination with transmyocardial laser revascularization, carotid endarterectomy, abdominal aortic aneurysm repair, lung surgery, gastrectomy (18) and is a well-described technique to shorten CPB and aortic cross clamp time for patients with coronary artery disease requiring combined valvular surgery (21).
Contraindications
In general, the small number of contraindications of off-pump CABG can be divided into absolute and relative (Table 2). Despite significant improvements in procedural performance, display of the target vessels in circumflex territory can be challenging, particularly in a patient with markedly impaired ejection fraction or when the surgeon is still in the early phase of his learning experience. Inability to expose the graftable vessels adequately translates into limited number of distal anastomoses and lack of complete revascularization.
Table 2
| Absolute contraindications |
| Cardiogenic shock |
| Major ischemic arrhythmias |
| Relative contraindications |
| Small, deep intramyocardial target vessels |
| Calcified target vessels |
| Poor ventricular function |
| Patients with deep pectus excavatum |
| Marked leftward displacement or rotation of the heart |
| Reoperation |
CABG, coronary artery bypass grafting. Reprinted with permission from Springer Nature Customer Service Centre GmbH: Raja SG. editor. Cardiac Surgery: A Complete Guide. Springer Nature, Copyright 2020. doi: https://doi.org/10.1007/978-3-030-24174-2.
Off-pump CABG due to manipulation-induced hemodynamic instability has a limited role in case of cardiogenic shock with a failing heart. In such a scenario, surgery using the CPB is inadvertent to avoid further deterioration of organ function (22). In the presence of widespread myocardial ischemia, cardiac failure and hemodynamic instability beating heart bypass surgery is best avoided.
Target vessels that are small in caliber, heavily atheromatous, or deep intramyocardial in location can account for incomplete revascularization (23). Coronary arteries with small caliber or heavy atheroma burden are challenging to graft even when CABG is performed using CPB on an arrested heart. Meticulous endarterectomy of heavily diseased coronary arteries should be carried out on-pump. Comprehensive dissection of an intramyocardial target vessel off-pump predisposes to danger of ventricular puncture and should be undertaken on-pump on a flaccid heart. Hybrid revascularization combining beating heart bypass surgery and coronary angioplasty can be a safer strategy in these challenging patients.
Technique
Off-pump multivessel grafting is performed through a standard median sternotomy (24). Median sternotomy offers the advantage of access to all potential targets, together with an unhindered approach to the left or right internal mammary artery for harvesting, and allows swift establishment of extracorporeal circulation should hemodynamic deterioration occur during off-pump CABG (18).
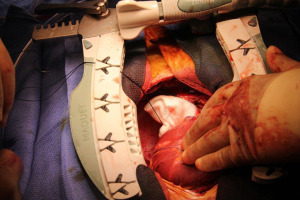
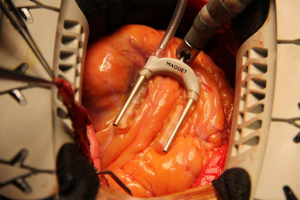
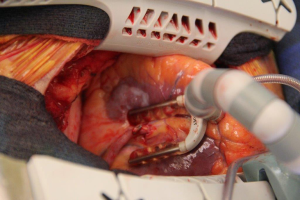
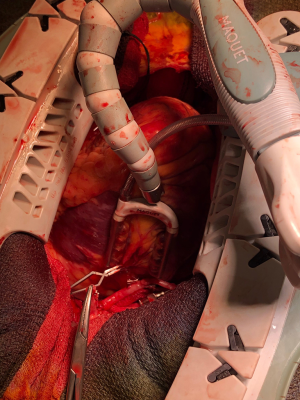
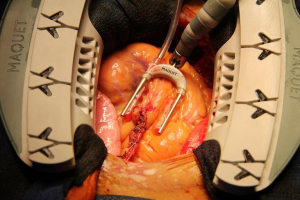
Dislocation of heart facilitates the exposure of coronary arteries on posterior, lateral, and inferior surfaces and can be accomplished either by the deployment of deep pericardial retraction sutures (Figure 1) or the use of stockinet sutured into the oblique sinus (25). Minimal displacement is required to display the LAD artery (Figures 2,3), its diagonal branches, or proximal right coronary artery (RCA) and can be achieved by positioning rolled large swabs in the pericardial cavity (26). Placement of pads, slings, pericardial sutures, or a retracting sock (18), either alone or in combination, are well-described strategies employed to improve the visibility of the circumflex artery (Figure 4), its branches, the posterior descending artery (Figure 5), and the posterolateral branch of the RCA. These aforementioned maneuvers luxate and elevate the heart anteriorly ensuring clear view of the target vessels on the inferior and lateral aspects.
Effective and localized stabilization of the anastomotic site enables seamless construction of a good quality anastomosis and is the key to successful off-pump grafting. Pressure or suction stabilizers positioned on the epicardium over the selected site of grafting minimize movement of the heart (18). This is a massive improvement from the early days, when reduction in heart rate was achieved with short-acting beta-blockers, diltiazem, or adenosine to create a relatively still anastomotic site (18). A variety of stabilizers have acquired approval with graft patency comparable to that of conventional CABG (27). Regional immobilization is achieved by positioning the stabilizer device on the myocardial surface over the selected spot for grafting.
A bloodless operative field is a fundamental requirement for safe construction of coronary anastomosis. An array of techniques including silastic snares or sutures, clamps, or coronary occluders have been utilized to create a bloodless operative field (18). These strategies also enable preconditioning if needed. Intravascular shunts are widely used due to their well-recognized benefits of preservation of coronary blood flow, avoidance of ischemia, diminished back bleeding, and visualization of suture line to prevent accidental suturing of the arterial back wall (28). Visualization is also improved by employing a surgical blower-mister that helps maintain moisture and increases visibility by gently displacing blood with a controlled flow of saline and carbon dioxide (29).
Anesthetic management
The fundamentals of anesthesia for off-pump surgery are similar to those for conventional on-pump surgery and involve safe induction and maintenance of general anesthesia with a strategy that offers utmost cardiac protection (18). Awareness of the coronary lesions, surgical strategy, and good communication between the surgeon and anesthesiologist is crucial (21). Avoidance and management of ischemia and hemodynamic instability during blockage of native coronary arteries, adequate postoperative pain relief, early emergence, extubation, and ambulation are important considerations. Prevention of hypothermia must be vigorously pursued (18). A cell saver may be utilized to lessen the requirement for homologous blood transfusion in multivessel beating heart bypass surgery. Transvenous pacing leads, defibrillator paddles, and provisions for intra-aortic balloon counterpulsation or emergency circulatory support should be available (18). Routine transesophageal echocardiography and cerebral oximetry are useful adjuncts for enhanced monitoring. Numerous interventions are employed to prevent hemodynamic deterioration and emergency conversion (Table 3).
Table 3
| Extensive right pleurotomy |
| Deep vertical right pericardiotomy |
| Gentle right decubitus Trendelenburg position |
| Ischemic preconditioning |
| Electrolyte optimization |
| Aggressive management of perfusion pressure |
| Constructing the proximal before the distal anastomosis |
| Revascularizing the territory of the LAD before lifting or turning the heart |
| Avoidance of surgery on the main RCA instead grafting its posterior descending branch |
| Pacing wires may be prophylactically sited in the right atrium or ventricle to overcome bradyarrhythmia |
| Prophylactic intra-aortic balloon pump placement for high-risk cases |
LAD, left anterior descending; RCA, right coronary artery. Reprinted with permission from Springer Nature Customer Service Centre GmbH: Raja SG. editor. Cardiac Surgery: A Complete Guide. Springer Nature, Copyright 2020. doi: https://doi.org/10.1007/978-3-030-24174-2.
There are diverse views with respect to the correct dose of heparin for beating heart bypass surgery, ranging from full heparinization to more moderate doses. It is generally believed that an activated coagulation time >300 seconds is acceptable, and this should be completely reversed upon completion of surgery with an adequate dose of protamine (18).
Outcomes
Since its resurgence, off-pump CABG has faced persistent criticism of skeptics. It has been intensely scrutinized with a massive increase in published research related to this technique over the last two decades. In fact, among techniques of coronary bypass surgery, beating heart bypass surgery is perhaps the most stringently evaluated modality (30). Abundant excellent quality evidence, in the form of large retrospective nonrandomized studies (31-35), single institutional RCTs (36-40) as well meta-analyses and systematic reviews (41-45) (Table 4), validates the status of off-pump CABG as a safe and effective technique. Similar outcomes have been reported for on-pump and off-pump CABG by the bulk of published outcomes research. However, erroneous interpretations about imperfect revascularization, diminished long-term graft patency and enhanced need for reintervention causing worse late survival (9) coupled with ineptitude of RCTs with inadequate sample size to exhibit significant differences in outcomes have encouraged antagonists of beating heart bypass surgery to call for a ban on this strategy (46). Opponents and critics of off-pump CABG are oblivious of the fact that larger retrospective studies (47-51) and recently conducted multi-institutional RCTs that are better powered to statistically compare outcomes have reported improved short-term results with off-pump CABG and comparable late outcomes (5-7,52,53) for both off- and on-pump CABG (Table 5).
Table 4
| Author, reference | Year | Studies included | Outcome(s) of interest | Number of patients | Key results |
|---|---|---|---|---|---|
| Filardo, (41) | 2018 | 42 RCTs, 31 obs | 30-day mortality; 5-year mortality; 10-year mortality | 1.2 million | RCTs showed no difference; combined analysis showed OPCAB offers lower short-term mortality but poorer long-term survival |
| Kowalewski, (42) | 2016 | 100 RCTs | All-cause mortality, MI, cerebral stroke | 19,192 | Same rate of all-cause mortality and MI Significant reduction in cerebral stroke rate with OPCAB |
| Luo, (43) | 2015 | 7 RCTs | Mortality, MI, stroke, renal failure, repeat revascularization | 9,128 | Similar outcomes except significantly higher revascularization rate with OPCAB |
| Chaudhry, (44) | 2014 | 5 RCTs, 5 RBS, 10 PMS, 12 obs | Mid and long-term survival, repeat revascularization, MI, stroke | 52,783 | Similar mid-term mortality and morbidity Improved long-term survival with ONCAB |
| Sedrakyan, (45) | 2006 | 41 RCTs | Mortality, stroke, wound infection, AF, repeat revascularization | 3,996 | Similar mortality; significantly reduced stroke, AF and wound infection rates with OPCAB; significantly increased repeat revascularization rate with OPCAB |
AF, atrial fibrillation; CABG, coronary artery bypass grafting; MI, myocardial infarction; Obs, observational studies; ONCAB, on-pump coronary artery bypass; OPCAB, off-pump coronary artery bypass; PMS, propensity-matched studies; RCT, randomized controlled trial; RBS, registry-based studies.
Table 5
| Trial, reference | 30-day mortality | Stroke | MI | Renal failure | Reoperation for bleeding | Similar index of completeness of revascularization | Repeat re-intervention | 1-year survival | 5-year survival |
|---|---|---|---|---|---|---|---|---|---|
| CORONARY trial, (5) | = | = | = | = | < | Yes | > | = | = |
| GOPCABE trial, (6) | < | < | < | < | < | No | NM | NA | NA |
| DOORS trial, (7) | = | = | = | = | = | Yes | NA* | NA | NA |
| ROOBY trial, (8) | = | = | = | = | = | No | > | < | < |
| On-off study, (52) | < | < | < | < | < | Yes | NM | NA | NA |
| The Best Bypass Surgery trial, (53) | = | = | = | = | = | Yes | = | NA | =+ |
<, less with off-pump CABG; >, more with off-pump CABG; =, same with off-pump & on-pump CABG; NA*, more graft occlusion with off-pump CABG; +, 3-year survival. CABG, coronary artery bypass grafting; MI, myocardial infarction; NA, not available; NM, not measured; RCTs, randomized controlled trials. Adapted with permission from Springer Nature Customer Service Centre GmbH: Raja SG. editor. Cardiac Surgery: A Complete Guide. Springer Nature, Copyright 2020. doi: https://doi.org/10.1007/978-3-030-24174-2.
In contemporary CABG practice referrals of patients with high-risk profile are on the rise. The advantages of off-pump CABG are evident for patients at high risk for complications attributed to CPB usage and aortic handling. Current publications have reported improved outcomes with off-pump CABG for higher-risk patients (52-56) (Table 6). Due to changing patient profile in the current era, off-pump CABG remains a beneficial strategy for patients considered high-risk for conventional CABG.
Table 6
| Author, reference | Year | Study type | Patient characteristics | Primary endpoint | Number (ONCAB, OPCAB) | Key outcomes |
|---|---|---|---|---|---|---|
| Lemma, (52) | 2012 | RCT | EuroSCORE ≥6 | Compositea | 195, 216 | Significantly more on-pump patients experienced primary end point |
| Møller, (53) | 2010 | RCT | EuroSCORE ≥5 | Compositeb | 176, 163 | No major differences |
| Barandon, (54) | 2008 | Case series | EuroSCORE >9 | Early mortality, ICU stay, MI, stroke, RRT | –120 | Early mortality 3%, ICU stay 2.7 days, MI 0.8%, stroke 0.8%, RRT 7% |
| Marui, (55) | 2012 | PSM | Division into tertile based on PROM | 30-day mortality, cardiovascular events | 1,377, 1,091 | Similar 30-day mortality, more 30-day stroke rate in high-risk ONCAB tertile |
| Vasques, (56) | 2013 | PSM | Age ≥80 years | Early mortality, ICU stay, MI, stroke, 5-year survival | 56, 56 | All outcomes similar except lower stroke rate with OPCAB |
a, Composite primary end point included operative mortality, MI, stroke, renal failure, reoperation for bleeding and adult respiratory distress syndrome within 30 days after surgery; b, composite of adverse cardiac and cerebrovascular events (i.e., all-cause mortality, acute MI, cardiac arrest with successful resuscitation, low cardiac output syndrome/cardiogenic shock, stroke, and coronary reintervention). CABG, coronary artery bypass grafting; RCT, randomized controlled trial; ICU, intensive care unit; MI, myocardial infarction; ONCAB, on-pump coronary artery bypass; OPCAB, off-pump coronary artery bypass; PROM, predicted risk operative mortality; RRT, renal replacement therapy; PSM, propensity score modeling.
Concerns
Occlusion of grafts is one of the key factors determining clinical prognosis after CABG. Substantial concern has been expressed by clinicians regarding the increasing technical complexity of off-pump coronary revascularization that might affect quality of anastomoses and graft patency (57). The 15-year patency rate for conventional on-pump CABG is >97%. Any new revascularization method must be compared against this benchmark (58). Inferior graft patency after off-pump CABG is attributed to a sharp learning curve, hindrance caused by cardiac movement or pulmonary excursions, and anastomotic suturing on a moving target (58).
Interestingly, majority of the concerns about suboptimal anastomotic quality and inferior graft patency over the years have been principally ascribed to two RCTs (8,59). Shroyer et al. (8) reported lower patency rate on 12-month angiography and higher composite adverse outcome rate (death from any cause, nonfatal MI, and any reintervention procedure) for off-pump than for on-pump CABG at 1 year. Limited surgical experience of 53 participating surgeons most likely accounted for the undesirable high conversion rates to on-pump CABG (12%) and lack of complete revascularization (18%) with poor outcomes for the off-pump CABG cohort. In addition, 60% of the cases were performed by relatively inexperienced residents which could have affected graft patency. Simultaneous utilization of endoscopic vein harvesting (EVH) in 1,471 patients (on-pump =907 and off-pump =564) in the Veterans Affairs (VA) Randomized On/Off Bypass (ROOBY) trial (8) was another potential confounder that impacted graft patency. On follow-up angiography, 41.3% patients in the EVH group had one or more occluded saphenous vein grafts compared with 28.0% in the open vein harvesting (OVH) group (P<0.0001). Overall patency of saphenous vein graft was markedly worse at 74.5% in the EVH group in comparison to 85.2% in the OVH group (P<0.0001) (60). Since ROOBY trial was enrolling at a time when practice of EVH was still in its infancy, the suboptimal vein graft patency due to EVH can be ascribed to learning curve and lack of experience of the vein harvesters. The learning curve for EVH results in poor conduit quality that has been held responsible for early graft failure, blunted positive remodeling, and greater negative remodeling (61).
The trial by Khan et al. (59) is the other frequently cited randomized trial that castigates off-pump CABG for poor graft patency. This trial reported decreased graft patency at 3 months in the off-pump group. However, critical analysis of this trial reveals that relative inexperience of the trial surgeons, comparatively low dose of intraoperative heparin, the lack of dual antiplatelet therapy usage postoperatively, and reliance on old fashioned stabilization devices with suboptimal exposure contributed to poor graft patency (4,62).
Controversies
Lack of complete revascularization due to fewer grafts is a controversy that has haunted off-pump CABG since its resurgence. The criticism regarding incomplete revascularization is no longer credible in the contemporary era due to availability of state of the art technology to safely perform multivessel off-pump CABG. Grafting of target vessels in the circumflex and RCA territories is not insurmountable any more. In fact, the more recently conducted randomized trials report at least comparable completeness of revascularization (5-7,52,53). Moreover, it is crucial to emphasize that completeness of revascularization and number of grafts are not synonymous. The index of completeness of revascularization [number of grafts performed divided by the number of grafts needed (number of graftable vessels with angiographically significant stenoses)] is a more rational way to deal with the controversy surrounding lack of complete revascularization (63).
The relative experience with each technique of the reporting center(s) and surgeon(s) influences revascularization rates reported by various studies comparing off-pump and on-pump CABG. Low volume off-pump CABG centers will report similar rates of complete revascularization in the early as well as late phases of off-pump experience emphasizing the significance of learning curve as well as case load. Contribution of cases from low volume off-pump centers can therefore influence the final completeness of revascularization rate reported by multicenter RCTs. The ROOBY trial illustrates this phenomenon (64). Nearly 4,000 isolated CABG procedures are performed annually in the VA system at 42 cardiac surgery facilities (65). During the enrollment phase of the ROOBY trial only 7 of the 42 centers could be rated as high-volume off-pump CABG centers because they performed at least 50 off-pump cases annually (66). As the learning curve for off-pump CABG is perceived to be between 50 and 75 cases (67) it does not come as a surprise that the ROOBY trial reports incomplete revascularization with off-pump CABG.
Long-term all-cause mortality is reported to be worse after off-pump CABG. Late mortality rates are negatively influenced by incomplete revascularization and lower graft patency (68). Takagi et al. (69) recently published a meta-analysis of 11 randomized trials comparing ≥1-year all-cause mortality after off-pump and on-pump CABG. Mortality was significantly increased by a factor of 1.37 with off-pump relative to on-pump CABG (RR: 1.373; 95% CI: 1.043–1.808). The ROOBY trial (8) emerged as a strong contributor to the pooled estimate as revealed by the sensitivity analysis in this meta-analysis. The inferior survival of off-pump cohort could be attributed to the previously mentioned criticisms of the ROOBY trial. It is important to mention that long-term outcomes, including late mortality data, for majority of the more contemporary trials (5-7,52,53) are still awaited.
It is anticipated that once information on long-term outcomes is available for contemporary RCTs (5-7,52-53), that deployed advanced technology for stabilization and exposure and had comparable index of completeness of revascularization for off-pump and on-pump CABG, these contentious issues will be addressed.
Conclusions
Despite abundant published evidence substantiating the benefits of off-pump CABG, apprehension prevails regarding the safety, effectiveness, and similarity of completeness of revascularization of off-pump CABG compared with on-pump CABG. Off-pump CABG is a challenging technique with a steep learning curve that accounts for all the concerns and controversies attributed to this technically demanding strategy. Appropriate patient selection, individualized grafting strategy, peer-to-peer training of the entire team, and graded clinical experience are some of the interventions that can facilitate safe negotiation of the learning curve of off-pump CABG. Off-pump CABG is an attractive strategy for treating high-risk patients and next generation of cardiac surgeons must receive structured training to perform off-pump CABG so as to deal with increasing numbers of high-risk patients that are being referred for surgical myocardial revascularization.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, AME Medical Journal for the series “Coronary Artery Bypass Grafting”. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj.2020.03.11/coif). The series “Coronary Artery Bypass Grafting” was commissioned by the editorial office without any funding or sponsorship. SGR served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of AME Medical Journal from September 2019 to September 2021.The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961-72. [Crossref] [PubMed]
- Raja SG, Benedetto U. Off-pump coronary artery bypass grafting: misperceptions and misconceptions. World J Methodol 2014;4:6-10. [Crossref] [PubMed]
- Raja SG. Two decades of off-pump coronary artery bypass surgery: Harefield experience. J Thorac Dis 2016;8:S824-8. [Crossref] [PubMed]
- Raja SG, Dreyfus GD. Current status of off-pump coronary artery bypass surgery. Asian Cardiovasc Thorac Ann 2008;16:164-78. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013;368:1179-88. [Crossref] [PubMed]
- Diegeler A, Börgermann J, Kappert U, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013;368:1189-98. [Crossref] [PubMed]
- Houlind K, Kjeldsen BJ, Madsen SN, et al. The impact of avoiding cardiopulmonary by-pass during coronary artery bypass surgery in elderly patients: the Danish On-pump Off-pump Randomisation Study (DOORS). Trials 2009;10:47. [Crossref] [PubMed]
- Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009;361:1827-37. [Crossref] [PubMed]
- Takagi H, Ando T, Mitta S, et al. Meta-analysis comparing ≥10-year mortality of off-pump versus on-pump coronary artery bypass grafting. Am J Cardiol 2017;120:1933-8. [Crossref] [PubMed]
- Vineberg AM, Niloff PH. The value of surgical treatment of coronary artery occlusion by implantation of the internal mammary artery into the ventricular myocardium; an experimental study. Surg Gynecol Obstet 1950;91:551-61. [PubMed]
- Bailey CP, May A, Lemmon WM. Survival after coronary endarterectomy in man. J Am Med Assoc 1957;164:641-6. [Crossref] [PubMed]
- Longmire WP Jr, Cannon JA, Kattus AA. Direct-vision coronary endarterectomy for angina pectoris. N Engl J Med 1958;259:993-9. [Crossref] [PubMed]
- Favaloro RG. Saphenous vein autograft replacement of severe segmental coronary artery occlusion: operative technique. Ann Thorac Surg 1968;5:334-9. [Crossref] [PubMed]
- Kolessov VI. Mammary artery-coronary artery anastomosis as method of treatment for angina pectoris. J Thorac Cardiovasc Surg 1967;54:535-44. [Crossref] [PubMed]
- Trapp WG, Bisarya R. Placement of coronary artery bypass graft without pump oxygenator. Ann Thorac Surg 1975;19:1-9. [Crossref] [PubMed]
- Ankeny JL. Editorial: To use or not to use the pump oxygenator in coronary bypass operations. Ann Thorac Surg 1975;19:108-9. [Crossref] [PubMed]
- Slogoff S, Keats AS. Does perioperative myocardial ischemia lead to postoperative myocardial infarction? Anesthesiology 1985;62:107-14. [Crossref] [PubMed]
- Raja SG, Dreyfus GD. Off-pump coronary artery bypass surgery: to do or not to do? Current best available evidence. J Cardiothorac Vasc Anesth 2004;18:486-505. [Crossref] [PubMed]
- Bakaeen FG, Shroyer AL, Gammie JS, et al. Trends in use of off-pump coronary artery bypass grafting: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. J Thorac Cardiovasc Surg 2014;148:856-3, 864.e1; discussion 863-4.
- Manoly I, Hasan R, Brazier A, et al. Feasibility of hybrid off pump artery bypass grafting and transaortic transcatheter aortic valveimplantation: a case series. Catheter Cardiovasc Interv 2017;89:1273-9. [Crossref] [PubMed]
- Raja SG, Husain M, Salhiyyah K, et al. Concomitant off-pump coronary artery bypass grafting results in improved in-hospital outcomes for patients with ischemic mitral regurgitation undergoing surgery. Heart Surg Forum 2013;16:E15-20. [Crossref] [PubMed]
- Hirose H, Amano A. Routine off-pump coronary artery bypass: reasons for on-pump conversion. Innovations (Phila) 2005;1:28-31. [Crossref] [PubMed]
- Czerny M, Baumer H, Kilo J, et al. Complete revascularization in coronary artery bypass grafting with and without cardiopulmonary bypass. Ann Thorac Surg 2001;71:165-9. [Crossref] [PubMed]
- Hirata N, Sawa Y, Takahashi T, et al. Is median sternotomy invasive? A comparison between minimally invasive direct coronary artery bypass and off-pump bypass. Surg Today 2000;30:503-5. [Crossref] [PubMed]
- Heames RM, Gill RS, Ohri SK, et al. Off-pump coronary artery surgery. Anaesthesia 2002;57:676-85. [Crossref] [PubMed]
- Soltoski P, Salerno T, Levinsky L, et al. Conversion to cardiopulmonary in off-pump coronary artery bypass grafting (Its effect on outcome). J Card Surg 1998;13:328-34. [Crossref] [PubMed]
- Subramanian VA. Less invasive arterial CABG on beating heart. Ann Thorac Surg 1997;63:S68-71. [Crossref] [PubMed]
- van Aarnhem EE, Nierich AP, Jansen EW. When and how to shunt the coronary circulation in off-pump coronary artery bypass grafting. Eur J Cardiothorac Surg 1999;16:S2-6. [Crossref] [PubMed]
- Sasaguri S, Hosoda Y, Yamamoto S. Carbon dioxide gas blow for the safe visualization of coronary artery anastomosis. Ann Thorac Surg 1995;60:1861. [PubMed]
- Raja SG. Safety of off-pump coronary artery surgery: no more skepticism please! Eur J Cardiothorac Surg 2004;26:1229. [Crossref] [PubMed]
- Kirmani BH, Holmes MV, Muir AD. Long-term survival and freedom from reintervention after off-pump coronary artery bypass grafting: a propensity-matched study. Circulation 2016;134:1209-20. [Crossref] [PubMed]
- Puskas JD, Kilgo PD, Lattouf OM, et al. Off-pump coronary bypass provides reduced mortality and morbidity and equivalent 10-year survival. Ann Thorac Surg 2008;86:1139-46. [Crossref] [PubMed]
- Hannan EL, Wu C, Smith CR, et al. Off-pump versus on-pump coronary artery bypass graft surgery: differences in short-term outcomes and in long-term mortality and need for subsequent revascularization. Circulation 2007;116:1145-52. [Crossref] [PubMed]
- Al-Ruzzeh S, Ambler G, Asimakopoulos G, et al. Off-pump coronary artery bypass (OPCAB) surgery reduces risk-stratified morbidity and mortality: a United Kingdom Multi-Center Comparative Analysis of Early Clinical Outcome. Circulation 2003;108:II1-8. [Crossref] [PubMed]
- Cleveland JC Jr, Shroyer AL, Chen AY, et al. Off-pump coronary artery bypass grafting decreases risk-adjusted mortality and morbidity. Ann Thorac Surg 2001;72:1282-8. [Crossref] [PubMed]
- van Dijk D, Nierich AP, Jansen EW, et al. Early outcome after off-pump versus on-pump coronary bypass surgery: results from a randomized study. Circulation 2001;104:1761-6. [Crossref] [PubMed]
- Puskas JD, Williams WH, Duke PG, et al. Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: a prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg 2003;125:797-808. [Crossref] [PubMed]
- Al-Ruzzeh S, George S, Bustami M, et al. Effect of off-pump coronary artery bypass surgery on clinical, angiographic, neurocognitive, and quality of life outcomes: randomised controlled trial. BMJ 2006;332:1365. [Crossref] [PubMed]
- Karolak W, Hirsch G, Buth K, et al. Medium-term outcomes of coronary artery bypass graft surgery on pump versus off pump: results from a randomized controlled trial. Am Heart J 2007;153:689-95. [Crossref] [PubMed]
- Noiseux N, Stevens LM, Chartrand-Lefebvre C, et al. Off-pump versus on-pump coronary artery bypass surgery: graft patency assessment with coronary computed tomographic angiography: a prospective multicenter randomized controlled pilot study. J Thorac Imaging 2017;32:370-7. [Crossref] [PubMed]
- Filardo G, Hamman BL, da Graca B, et al. Efficacy and effectiveness of on- versus off-pump coronary artery bypass grafting: a meta-analysis of mortality and survival. J Thorac Cardiovasc Surg 2018;155:172-9.e5. [Crossref] [PubMed]
- Kowalewski M, Pawliszak W, Malvindi PG, et al. Off-pump coronary artery bypass grafting improves short-term outcomes in high-risk patients compared with on-pump coronary artery bypass grafting: meta-analysis. J Thorac Cardiovasc Surg 2016;151:60-77.e1-58.
- Luo T, Ni Y. Short-term and long-term postoperative safety of off-pump versus on-pump coronary artery bypass grafting for coronary heart disease: a meta-analysis for randomized controlled trials. Thorac Cardiovasc Surg 2015;63:319-27. [Crossref] [PubMed]
- Chaudhry UA, Harling L, Rao C, et al. Off-pump versus on-pump coronary revascularization: meta-analysis of mid- and long-term outcomes. Ann Thorac Surg 2014;98:563-72. [Crossref] [PubMed]
- Sedrakyan A, Wu AW, Parashar A, et al. Off-pump surgery is associated with reduced occurrence of stroke and other morbidity as compared with traditional coronary artery bypass grafting: a meta-analysis of systematically reviewed trials. Stroke 2006;37:2759-69. [Crossref] [PubMed]
- Lazar HL. Should off-pump coronary artery bypass grafting be abandoned? Circulation 2013;128:406-13. [Crossref] [PubMed]
- Mack MJ, Pfister A, Bachand D, et al. Comparison of coronary bypass surgery with and without cardiopulmonary bypass in patients with multivessel disease. J Thorac Cardiovasc Surg 2004;127:167-73. [Crossref] [PubMed]
- Zangrillo A, Crescenzi G, Landoni G, et al. Off-pump coronary artery bypass grafting reduces postoperative neurologic complications. J Cardiothorac Vasc Anesth 2005;19:193-6. [Crossref] [PubMed]
- Farrokhyar F, Wang X, Kent R, et al. Early mortality from off-pump and on-pump coronary bypass surgery in Canada: a comparison of the STS and the EuroSCORE risk prediction algorithms. Can J Cardiol. 2007;23:879-83. [Crossref] [PubMed]
- Racz MJ, Hannan EL, Isom OW, et al. A comparison of short- and long-term outcomes after off-pump and on-pump coronary artery bypass graft surgery with sternotomy. J Am Coll Cardiol. 2004;43:557-64. [Crossref] [PubMed]
- Gobran SR, Goldman S, Ferdinand F, et al. Outcomes after usage of a quality initiative program for off-pump coronary artery bypass surgery: a comparison with on-pump surgery. Ann Thorac Surg. 2004;78:2015-21. [Crossref] [PubMed]
- Lemma MG, Coscioni E, Tritto FP, et al. On-pump versus off-pump coronary artery bypass surgery in high-risk patients: operative results of a prospective randomized trial (on-off study). J Thorac Cardiovasc Surg 2012;143:625-31. [Crossref] [PubMed]
- Møller CH, Perko MJ, Lund JT, et al. No major differences in 30-day outcomes in high-risk patients randomized to off-pump versus on-pump coronary bypass surgery: the best bypass surgery trial. Circulation 2010;121:498-504. [Crossref] [PubMed]
- Barandon L, Richebé P, Munos E, et al. Off-pump coronary artery bypass surgery in very high-risk patients: adjustment and preliminary results. Interact Cardiovasc Thorac Surg 2008;7:789-93. [Crossref] [PubMed]
- Marui A, Okabayashi H, Komiya T, et al. Benefits of off-pump coronary artery bypass grafting in high-risk patients. Circulation 2012;126:S151-7. [Crossref] [PubMed]
- Vasques F, Rainio A, Heikkinen J, et al. Off-pump versus on-pump coronary artery bypass surgery in patients aged 80 years and older: institutional results and meta-analysis. Heart Vessels 2013;28:46-56. [Crossref] [PubMed]
- Raja SG, Dreyfus GD. Impact of off-pump coronary artery bypass surgery on graft patency: current best available evidence. J Card Surg 2007;22:165-9. [Crossref] [PubMed]
- Cooley DA. Con: beating-heart surgery for coronary revascularization: is it the most important development since the introduction of the heart-lung machine? Ann Thorac Surg 2000;70:1779-81. [Crossref] [PubMed]
- Khan NE, De Souza A, Mister R, et al. A randomized comparison of off-pump and on-pump multivessel coronary-artery bypass surgery. N Engl J Med 2004;350:21-8. [Crossref] [PubMed]
- Zenati MA, Shroyer AL, Collins JF, et al. Impact of endoscopic versus open saphenous vein harvest technique on late coronary artery bypass grafting patient outcomes in the ROOBY (Randomized On/Off Bypass) Trial. J Thorac Cardiovasc Surg 2011;141:338-44. [Crossref] [PubMed]
- Raja SG, Sarang Z. Endoscopic vein harvesting: technique, outcomes, concerns & controversies. J Thorac Dis 2013;5:S630-7. [PubMed]
- Dewey TM, Magee MJ, Mack MJ. Off-pump versus on-pump coronary bypass surgery. N Engl J Med 2004;350:1791-3; author reply 1791-3.
- Magee MJ, Hebert E, Herbert MA, et al. Fewer grafts performed in off-pump bypass surgery: patient selection or incomplete revascularization? Ann Thorac Surg 2009;87:1113-8. [Crossref] [PubMed]
- Hattler B, Messenger JC, Shroyer AL, et al. Off-Pump coronary artery bypass surgery is associated with worse arterial and saphenous vein graft patency and less effective revascularization: results from the Veterans Affairs Randomized On/Off Bypass (ROOBY) trial. Circulation 2012;125:2827-35. [Crossref] [PubMed]
- Bakaeen FG, Chu D, Kelly RF, et al. Performing coronary artery bypass grafting off-pump may compromise long-term survival in a veteran population. Ann Thorac Surg 2013;95:1952-8; discussion 1959-60.
- Bakaeen FG, Kelly RF, Chu D, et al. Trends over time in the relative use and associated mortality of on-pump and off-pump coronary artery bypass grafting in the Veterans Affairs system. JAMA Surg 2013;148:1031-6. [Crossref] [PubMed]
- Patel NN, Angelini GD. Off-pump coronary artery bypass grafting: for the many or the few? J Thorac Cardiovasc Surg 2010;140:951-3.e1. [Crossref] [PubMed]
- Bell MR, Gersh BJ, Schaff HV, et al. Effect of completeness of revascularization on long-term outcome of patients with three-vessel disease undergoing coronary artery bypass surgery. A report from the Coronary Artery Surgery Study (CASS) Registry. Circulation 1992;86:446-57. [Crossref] [PubMed]
- Takagi H, Matsui M, Umemoto T. Off-pump coronary artery bypass may increase late mortality: a meta-analysis of randomized trials. Ann Thorac Surg 2010;89:1881-8. [Crossref] [PubMed]
Cite this article as: Marczin N, Raja SG. Off-pump coronary artery bypass grafting. AME Med J 2020;5:21.