
Pyoderma gangrenosum in ulcerative colitis
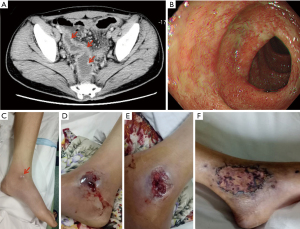
A 21-year-old man presented to an outpatient clinic with an 8-month history of hematochezia, abdominal pain, tiredness, and weight loss. His abdomen was soft, with mild left lower quadrant abdominal tenderness and active bowel sounds. Laboratory evaluation revealed a hemoglobin level of 10.4 g per deciliter (normal range, 13.5 to 17.5). Computed tomography of the abdomen revealed thickened wall of colon sigmoideum and rectum (Figure 1A). The colonoscopy showed congestion, edema and ulcer in the same location (Figure 1B), and mucosal biopsy by colonoscopy suggested that submucosal abscess was formed and presented as fissuring ulcers. T-SPOT.TB assay was negative. Two weeks later, the painful and rapidly progressive ulcerative lesions involving the left ankle joint was shown sequentially accompanied by red swollen (the 1st day; Figure 1C), deep ulcers (the 3rd day; Figure 1D), and necrosis (the 5th day; Figure 1E). The physical examination showed skin ulcerations with both an irregular purple and a purulent base edge. The histopathological detection of an incisional biopsy sample separated from the ankle lesion revealed both superficial dermal and epidermal necrosis with leukocytoclastic vasculitis, an underlying mixed inflammatory-cell infiltrate and abscess formation. Direct microbiologic detection and cultures were negative for bacterial and fungal pathogens. A diagnosis of pyoderma gangrenosum (PG) in ulcerative colitis was made. PG is an inflammatory skin disease with characteristics of rarity, chronicity and destructiveness, in which a painful nodule or pustule breaks down to generate a progressive and expansive ulcer with a undermined, tender and raised border (1-3). PG is usually related to systemic proinflammatory states, most particularly inflammatory bowel disease (4,5). Treatment can be extremely challenging, usually involving different kinds of immunosuppressive therapies (6,7). In this patient, the debridement was given. Treatment with sulfasalazine was initiated, and 2 weeks later, methylprednisolone therapy was started. Four weeks later, dermatoplasty was performed. The cutaneous ulcers had diminished substantially, with residual superficial atrophic scars on the 7th day after the operation (Figure 1F). He was discharged home with synchronous resolution of hematochezia and abdominal pain symptoms, as well as with outpatient follow-up.
Acknowledgments
Funding: This work was supported by National Natural Science Foundation of China (No.31600134).
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj-20-23/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this study and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Neil Crowson A. C. Mihm Jr M, Magro C. Pyoderma gangrenosum: a review. J Cutan Pathol 2003;30:97-107. [Crossref]
- Wollina U. Pyoderma gangrenosum–a review. Orphanet J Rare Dis 2007;2:19. [Crossref] [PubMed]
- Ruocco E, Sangiuliano S, Gravina A, et al. Pyoderma gangrenosum: an updated review. J Eur Acad Dermatol Venereol 2009;23:1008-17. [Crossref] [PubMed]
- Inayat F, Hurairah A. Pyoderma Gangrenosum at a Rare Site in Crohn’s Disease. Clin Gastroenterol Hepatol 2016;14:e75-6. [Crossref] [PubMed]
- Plumptre I, Knabel D, Tomecki K. Pyoderma Gangrenosum: a review for the gastroenterologist. Inflamm Bowel Dis 2018;24:2510-7. [Crossref] [PubMed]
- Ahn C, Negus D, Huang W. Pyoderma gangrenosum: a review of pathogenesis and treatment. Expert Rev Clin Immunol 2018;14:225-33. [Crossref] [PubMed]
- Alavi A, French LE, Davis MD, et al. Pyoderma gangrenosum: an update on pathophysiology, diagnosis and treatment. Am J Clin Dermatol 2017;18:355-72. [Crossref] [PubMed]
Cite this article as: Zeng MY, Liu W. Pyoderma gangrenosum in ulcerative colitis. AME Med J 2021;6:32.

