Choroidal tubercles as harbinger for miliary tuberculosis
Tuberculosis is rampant in Southeast Asia. Miliary Koch’s is a disseminated form of tuberculosis due to hematogenous spread of tuberculosis to lungs, liver and other systems which accounts for less than 2% of all tuberculosis cases. Patient’s symptoms usually range from nonspecific constitutional symptoms in form of fever, generalized weakness, weight loss, lassitude, cough, shortness of breath, headache and altered sensorium. Choroid tubercle, one of the pathogenomic features of miliary tuberculosis, can be detected early with a fundus examination and may help in initiating antitubercular therapy.
This patient aged 27 years had subacute illness of headache for the last one month for which she was taking analgesics. There was no nausea, vomiting, seizure or any history of altered sensorium. There was undocumented history of mild fever with preserved appetite. A month later, she came with unbearable headache nor any history of blurring of vision nor diplopia. Patient did not have any history of previous tuberculosis or any other comorbidities.
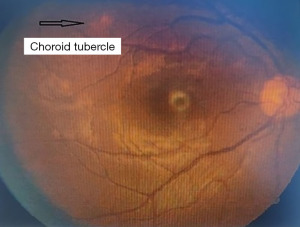
Patient was vitally stable with normal general physical examination. Central nervous system (CNS) examination showed terminal neck rigidity without any motor, sensory nor autonomic deficit. All cranial nerves were normal, other systemic examinations were within normal limits. Patient’s investigation revealed hemoglobin 10.9, erythrocyte sedimentation rate (ESR) 32, Mantoux test were positive with length and breadth of 10 mm × 15 mm; peripheral smear had microcytic hypochromic red blood cells. Whole abdomen ultrasonography was within normal limit; other biochemical investigation, including hepatitis B surface antigen (HbsAg), anti-hepatitis C virus, human immunodeficiency virus, serum Widal, Malaria card test and NS1Ag was within normal limit. Chest X-ray (CXR) revealed millet seed sized tubercles as shown in Figure 1. Cerebrospinal fluid (CSF) analysis revealed raised proteins, reduced glucose level and raised lymphocytes which suggested possibility of tubercular meningitis. Fundus examination revealed clear bilateral eye media with cup disc ratio of 0.3:1 and arteriovenous ratio (AVR) 2:3 foveal reflux was presented with well-defined disc margin. Multiple choroid tubercles were seen on posterior pole and there was no papilledema (Figure 2). Non-contrast computed tomography (NCCT) head was normal.
We would like to have a definitive diagnosis of tuberculosis. However, the patient declined for any invasive intervention, as she had neither any fulminant tuberculosis symptoms nor ocular symptoms. Therefore, we diagnosed this patient clinicoradiologically as a case of disseminated tuberculosis for having atypical presentation of headache and supported with radiological and ocular evidence of tuberculosis with choroid tubercle as shown in Figure 2 and having millet seed sized tubercular foci shadows as shown in Figure 1.
As the disease can rapidly deteriorate, we started the antitubercular therapy in the dose of Tablet (Tab) isoniazid 250 mg once daily, Tab. rifampicin 450 mg once daily, Tab ethambutol 800 mg once daily, Tab pyrazinamide 1,200 mg once daily along with steroids in the dose of Tab Dexamethasone 8 mg three times a day following with tapering weekly. The patient responded to the treatment and in the follow up after 8 weeks, she was asymptomatic. Repeating fundus examination at this point showed disappearing choroid tubercles (Figure 3).
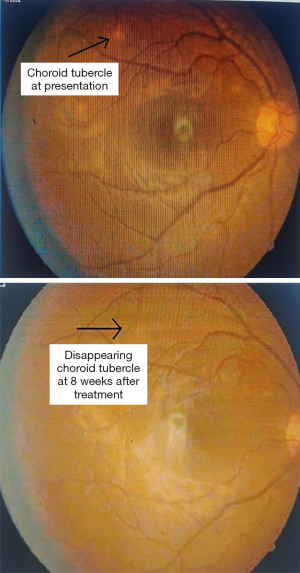
Disseminated tuberculosis may not classically present with its florid presentation of weight loss, cachexia or cough and fever. Headache may be the only manifested symptom and examination of eye provides vital clue for its diagnosis in the form of choroid tubercles. Timely diagnosis and subsequent treatment of tuberculosis prevented complications in this case and patient improved both clinically and radiologically which can be appreciated in form of regression of choroid tubercle.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://amj.amegroups.com/article/view/10.21037/amj-23-4/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj-23-4/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this “Images in Clinical Medicine”.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Cite this article as: Yadav P, Aggarwal R, Ghotekar LH. Choroidal tubercles as harbinger for miliary tuberculosis. AME Med J 2023;8:30.