The hip spine relationship—what we know and what we don’t: a narrative review
Introduction
The connection between the spine, pelvis, and hips is essential for functional movement, stability, and posture. This interplay between the lumbar spine and the pelvis, which encompasses bones, joints, muscles, ligaments, and other structures, has been referred to as the lumbopelvic complex (LPC) (1). Maintaining proper alignment, strength, and coordination of the LPC is important for optimizing function and promoting overall musculoskeletal health as this region serves as the major connection and stabilizer of the upper and lower halves of the body. If one aspect of the system becomes dysfunctional or imbalanced, it can affect other areas of the complex, leading to pain and disability. Depending on which pathology dominates the clinical pictures, concurrent degenerative pathologies in the hip and spine are referred to as hip-spine syndrome (HSS) or spine-hip syndrome (SHS) (2). Understanding the intricate relationships that exist between these structures when evaluating patients with LPC pathology is essential to optimize their outcomes.
The literature is unclear whether postoperative outcomes are optimized if lumbar fusions or hip arthroplasty is the index surgery. This is complicated based on the nature of the lumbar spine procedure given that single- or two-level procedures in the upper lumbar spine are less rigid and have less influence on pelvic parameters than multi-level fusions extended to the pelvis. Previous reviews have commented on the timing of these procedures (2,3), but we aimed to integrate new radiographic parameters into the conversation of surgical decision-making in these patients. Therefore, the objective of this article is to provide a review of the current literature on the hip-spine relationship as well as discuss its clinical importance in candidates for surgery. We present this article in accordance with the Narrative Review reporting checklist (available at https://amj.amegroups.com/article/view/10.21037/amj-23-163/rc).
Methods
A literature review was conducted via the PubMed database. Articles were screened based on their relevancy, recency, and quality of analysis. To establish spinopelvic parameters, articles and studies that provided the foundation for these parameters were included, with the oldest article published in 2005. Updates to parameters and their utility in clinical practice were preferentially searched between 2017–2023. Reviews, retrospective cohort studies, and retrospective case-control studies were all considered for inclusion. Animal studies were excluded from this review. Our literature review search was conducted on May 03 2023. Search items included the following MeSH terms: “lumbar spine” with free text items: “hip, arthroplasty, parameters, spinopelvic, sagittal alignment, fusion, total hip arthroplasty, hip-spine syndrome, surgical complications, and dislocation”. This search was carried out independently by one of the authors (M.M.) (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | May 03 2023 |
| Databases searched | PubMed |
| Search items used | MeSH: lumbar spine |
| Free text search terms: hip, arthroplasty, parameters, spinopelvic, sagittal alignment, fusion, total hip arthroplasty, hip-spine syndrome, surgical complications, dislocation | |
| Timeframe | January 01 2005–May 03 2023 |
| Inclusion and exclusion criteria | Inclusion: retrospective cohort, retrospective case control, reviews |
| Exclusion: animal studies | |
| Selection process | Search and selection was conducted independently by one of the authors (M.M.) |
MeSH, Medical Subject Headings.
Spinopelvic parameters
General alignment principles dictate that the spine, pelvis, and hip function together to maintain proper balance. A conceptual model described as the “cone of economy”, first introduced by Dubousset in the 1970s, is based on a cone-shaped structure, originating from the feet of a person in a standing position and expanding upward and outward (4). This cone represents the range of postures in which the body can maintain balance with minimal effort and without external support. As we move toward the outer edges of the cone, maintaining balance requires greater muscle activation, effort, and energy expenditure. Once we move beyond these edges, external support aids such as canes or walkers may be necessary. Changes in any component of the spine, pelvis, or hip can alter how an individual stands within the cone of economy, and if unfixed, can result in pain or disability (5).
Several parameters have been developed and verified to evaluate spinal alignment. Principles of alignment include preservation of cervical lordosis, thoracic kyphosis, and lumbar lordosis (LL) (6). Maintaining a neutral spine helps distribute forces evenly and minimizes stress on spinal structures (7). The sagittal vertical axis (SVA), one parameter used to assess alignment, quantifies the deviation of the spine from a plumb line in the sagittal plane. A plumb line refers to a vertical line drawn downwards to represent vertical gravitational force acting on the body. The SVA is determined by measuring the distance between the plumb line from the C7 vertebrae and the posterior superior corner of the S1 vertebral body (Figure 1A). Spinal alignment can also be assessed similarly in the coronal plane by measuring the distance between the C7 plumb line and the central sacral vertical line (CSVL) (Figure 1B) (5).
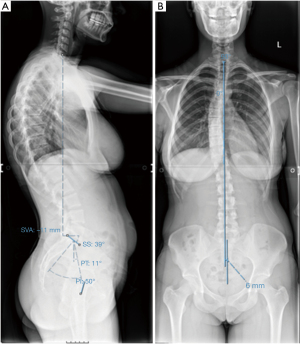
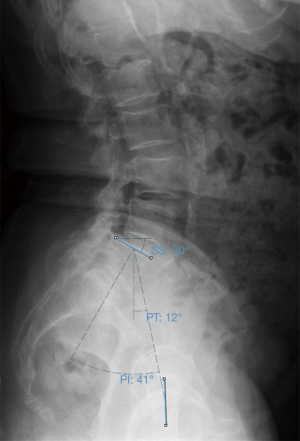
The pelvis also plays a role in maintaining the sagittal alignment as it serves as a link between the lumbar spine and hips. Spinopelvic alignment is typically evaluated using three parameters: pelvic tilt (PT), sacral slope (SS), and pelvic incidence (PI) (Figure 2). PT is defined as the angle created by a line drawn from the midpoint of the sacral endplate to the center of the bicoxofemoral axis and a vertical plumb line extending upwards from the bicoxofemoral axis. SS is measured as the angle created by a line drawn along the end plate of the sacrum and a horizontal reference line drawn from the posterior superior corner of S1 (5). PI is the sum of these two angles (PI = PT + SS) and is representative of the angle generated between a line drawn from the center of the femoral head to the sacral endplate and a line drawn orthogonally to the sacral endplate. PI is an independent fixed parameter that remains constant once an individual reaches skeletal maturity. Due to the fixed nature of PI, postural changes such as sitting or standing will only alter SS and PT, as these are dynamic parameters that describe the orientation of the pelvis in different positions or activities. The normal ranges for PI, PT, and SS have been shown to be 53°±11°, 0–15°, and 30°–45°, respectively. Notably, SS decreases to an average of 20° when seated (8,9).
The anterior pelvic plane (APP) represents the orientation and alignment of the pelvis in the sagittal plane and is another commonly used pelvic parameter. It is defined by three anatomical reference points: the two anterosuperior iliac spines and the anterior surface of the pubic symphysis. By connecting these three points, the APP is formed (Figure 3) (10). The ante-inclination (AI) angle, in the context of the acetabulum or cup in the case of a total hip arthroplasty (THA), can be defined as the combined measurement of both anteversion and inclination, representing the sagittal angle of the hip joint (9).
While in motion, the hip, spine, and pelvis move in constant coordination. As we transition from a seated to a standing position, the spinopelvic relationship undergoes the following changes to maintain sagittal balance: the lumbar spine increases in lordosis with the pelvis undergoing anteversion. This then leads to increased SS and decreased PT. When moving from a standing position to a seated position, the opposite occurs with the flexion of the lumbar spine and retroversion of the pelvis leading to decreased SS and increased PT (11).
The abnormal hip-spine relationship
The relationship between the spine, pelvis, and hips plays a crucial role in maintaining proper alignment and balance; however, abnormalities in this relationship can occur, leading to various musculoskeletal conditions and functional impairments. While the mechanisms above describe temporary changes in postural alignment that occur during normal movements, patients with prolonged misalignment can develop long-term characteristic changes.
As part of the normal degenerative process seen with ageing, patients progressively develop degenerative disc disease which often manifests as a loss of LL. Subsequent compensation results in decreases in SS and increased pelvic retroversion in order to keep a neutral sagittal balance. The pelvic retroversion is then compensated for with hip extension, and the combination of these factors leads to the functional anteversion of the acetabulum (5,12). This is of special concern in patients requiring THA as this heightens the risk of posterior impingement and anterior dislocation due to insufficient coverage of the femoral head and can correlate with higher failure rates due to excessive wear and implant instability, as one case series found 7/9 (78%) of patients that experienced anterior dislocation had hip hyperextension and fixed posterior PT (13).
As sagittal misalignment progresses, compensatory mechanisms evolve and eventually will reach their own limitations, thus marking the transition to the decompensated stage. Compensatory mechanism failure can result in two distinct syndromes. HSS occurs when hip pathology leads to the development of spinal symptoms, while SHS develops when lumbopelvic pathology contributes to hip dysfunction (10). During the decompensated stage, patients are unable to return within the cone of economy through normal compensatory mechanisms and must flex their knees and/or ankles or use balance aids to maintain sagittal alignment and forward gaze. Prolonged exposure outside of the cone of economy is not only energy intensive, but also painful.
Hip-spine parameters after surgery
Lumbar fusion may lead to a reduction in LL, often referred to as a “flat back”. This loss of lordosis leads to compensatory pelvic retroversion to maintain forward gaze, leading to decreased SS and increased PT. These changes deviate from the normal expected values for the same PI. One study found significantly higher rates of adjacent segment disease (ASD) in patients with an anterior C7 plumb line (50%) and decreased SS (47.8%) when compared to patients with a normal C7 plumb line and SS (8%) (14). A review by Le Huec and colleagues found it is important to assess the necessary LL for optimal sagittal balance prior to surgery, especially in patients with a high PI (15). Compensatory mechanisms for LL loss tend to reverse after successful surgery; however, the correction should be proportional to the PI value to achieve the desired outcomes, with postoperative improvement in PT suggesting a favorable clinical prognosis.
Degenerative hip disorders often coexist with degenerative changes of the lumbar spine, as evidenced by an increasing number of patients undergoing both THA and lumbar spinal fusion procedures (approximately 2% of patients undergoing THA have had a prior lumbar spinal fusion) (16,17). While spine surgery can provide stability and improve alignment parameters, it also impacts hip mechanics. After spinal fusion, the ability for the body to adjust the version of the pelvis becomes limited. Lazennec et al. (18) observed minimal change in cup anteversion and inclination when transitioning from standing to sitting, which has since been replicated (19). Mancino et al. also showed that in the presence of spinal stiffness, which can occur from degenerative disease or spinal fusion, pelvis movement is limited and does not allow appropriate anteversion to accommodate hip flexion. This can result in a seated position with relative acetabular retroversion, which increases the risk of anterior impingement, putting the patient at risk for posterior dislocation (10). Multilevel fusion can further increase functional acetabular retroversion when compared to single-level fusions, further increasing this risk (18).
When managing patients with previous fusion or spinal stiffness, adult reconstruction surgeons should carefully consider orientation of the acetabular component (19). Ukai et al. retrospectively compared spinal parameters in patients with and without spinal fusion. They found that after surgery, patients in the fusion group had a higher SVA compared to those in the non-fusion group. The fusion group also had a higher PT as compared to the non-fusion group. Additionally, several studies found a positive correlation between length of fusion and the rate of joint space narrowing after surgery, highlighting an increased risk of progression to osteoarthritis with multilevel spine fusion due to altered loading patterns (standardized beta coefficient: 0.374, P<0.0001) (20,21).
Much like the impact fusion can have on THA, hip arthroplasty can also affect spine kinematics. Kim et al. observed a notable association between hip mobility in four distinct positions (free-standing, extension, relaxed-seated, and flexed-seated) and changes in pelvic mobility, as defined by ΔSS, preoperatively and one year after undergoing primary THA in a population of 165 patients indicated for THA in Japan without scoliosis >25° or prior fusion >2 levels. The authors also discovered a significant decrease in pelvic (ΔSS standing to flexed-seated: 10° change, P<0.001) and lumbar (ΔLL standing to flexed-seated: 7° change, P<0.001) mobility one year after THA, while hip mobility experienced a considerable increase (22). PI-LL mismatch was not significantly different preoperatively and at one-year follow-up. Though this study was conducted in a small, specific population, the control for surgical variance by observing patients of a single spine surgeon using a consistent, modified anterolateral approach strengthens the study’s internal validity.
THA and lumbar fusion
THA remains one of the most commonly performed orthopedic procedures, boasting an excellent success rate and increased projections of future case load (10). Postoperative instability and dislocations are the most common complications for adult reconstruction surgeons. To mitigate risk, surgeons employ various strategies, including careful preoperative planning, advanced surgical techniques to optimize implant stability, and rigorous rehabilitation protocols.
Dislocations have been shown to be multifactorial, and recent literature supports evidence that spinopelvic abnormalities, such as decreased mobility, may play a role. Gausden et al. found that inflammatory arthritis, avascular necrosis, depression, lower socioeconomic status, and discharge to a skilled nursing facility were identified as independent risk factors for dislocations (23). They also found that a previous spinal fusion was the most significant independent predictor of dislocation within the first 6 months, and the adjusted odds of dislocation in spinal fusion patients were over twice that of dislocation in patients without prior spinal fusion [odds ratio (OR) =2.45]. Notably, this study used a national database that did not contain known confounders of dislocation, such as surgeon volume, surgical approach, or soft tissue repair. The occurrence of dislocation is notably higher, up to 5–10 times more, among individuals with spinal deformities (10). A retrospective study of dislocations after primary hip arthroplasty observed greater posterior PT (56.6° vs. 59.5°, P=0.02) in patients who had a dislocation when compared to matched controls, further highlighting the impact spinopelvic parameters can have on complications in this patient population (24). This has sparked growing attention towards studying the abnormalities in hip-spine motion and their influence on the outcomes of THA.
Malkani et al. also showed that lumbar fusion before THA is an independent risk factor for dislocation leading to increased risk of revision (16). The authors observed an 80% increase in dislocation in the fusion group at 6 months, 71% at 1 year, and 60% at 2 years. Interestingly, patients that had undergone fusion procedures were not the only cohort of patients at increased risk of dislocation; patients with spine disease that had not undergone fusion were also at an increased risk of dislocation when compared to controls (25). This study also could not control for surgical approach as it was a review of the Medicare part B claims database. Bernstein et al. found that the number and location of levels fused were also significant factors of post-operative mobility. Patients with previous L5–S1 fusion were found to have the greatest decreased pelvic mobility and arc of motion, indicating the potential for higher risk of dislocation (19).
Given the observed increased rate of dislocation seen in patients with THA and lumbar fusion, some speculated that timing of the procedures may impact dislocation rates as well (26). Bala et al. evaluated two cohorts: patients who underwent THA with subsequent lumbar fusion and patients who had lumbar fusion with subsequent THA. Increased dislocation rates were observed in both groups compared to controls; however, dislocation rates were significantly lower in patients who underwent THA first (1.7% vs. 4.6%, P<0.001). The authors theorized a patient’s THA may remain stable and function well due to a properly positioned acetabular implant in an already stiff, immobile spine. The subsequent correction of LL during lumbar fusion may not significantly change functional anteversion, causing no increase in the risk of dislocation (26). Another study observed similar findings, noting significantly higher risk of dislocation with previous spinal fusion in THA patients when compared to THA followed by delayed fusion (27). Conversely, Yang et al. observed the opposite, finding that patients who undergo THA prior to lumbar fusion have a significantly increased risk of postoperative dislocation (OR =2.46, P<0.0001), infection (OR =2.65, P<0.0001), revision surgery (OR =1.91, P<0.0001), and prolonged opioid use (OR =3.28, P<0.001) compared with THA after fusion (28). These differences may be in part explained by evaluation of different patient populations. Yang et al. studied patients privately insured with data extracted from the PearlDiver database, while Malkani et al. and Bala et al. studied Medicare patients. Additionally, Yang et al. utilized a regression model that controlled for age, sex, race, and Charlson Comorbidity Index (CCI). Malkani et al. controlled for additional factors such as census region, year THA was performed, pre-existing conditions, discharge status, length of stay, and various hospital characteristics in their multivariate regression. None of the studies were able to verify surgical approach due to the use of databases that do not code that information, a limitation in all three studies.
Another factor that may affect outcomes is the heterogeneity of approach in THA in patients with spinal fusion. Goyal et al. investigated direct anterior versus direct lateral approaches for THA and found no difference between the two approaches, perhaps due to the overall low dislocation rate (n=5, 0.9%) (29). Interestingly, in this study, no differences were noted in a sub analysis that compared the timing of the two procedures as well. Another study that compared posterior and anterior approaches in patients with lumbar spondylosis or previous lumbar fusion found a 4× increased risk of dislocation in patients undergoing posterior approach THA (OR =4.7, P=0.002) (30). Notably, the radiographic parameters, such as cup version and inclination, were not controlled for in the study. A more recent study comparing these two approaches supported these findings, showing prior instrumented fusion was not associated with increased dislocation risk in patients receiving an anterior approach (31). This study also had some significant limitations, including a greater proportion of anterior approach hips having dual mobility implants, which may favor stability.
Sultan et al. presented an algorithm on how to manage this patient population who have both hip osteoarthritis and adult spinal deformity (32). Upon initial consultation, it is important to evaluate for a hip flexion contracture. Addressing hip flexion contractures may help correct spine alignment issues and promote achievement of sagittal balance. Thus, these patients should undergo THA first, and their sagittal balance should be subsequently evaluated and addressed as needed. In patients without hip flexion contractures, they recommended addressing the more symptomatic region first. In patients who initially undergo spine deformity correction and need subsequent THA, Phan et al. proposed recommendations for optimal cup position in these patients that differ slightly from the traditional ‘safe zones’, defined as acetabular inclination between 30° and 50° and anteversion angle between 5° and 25° (33,34). The author recommends placement of the acetabular cup closer to the upper range of the safe zone to compensate for increased retroversion in the seated position, while maintaining normal standing range of motion (33). Monitoring pre-existing spine deformity progression after THA is a key component of follow-up to ensure the patient does not also need a lumbar fusion procedure for alignment correction. These recommendations can guide surgeons in determining the appropriate management of patients who need both THA and spine realignment.
Outcomes after THA and lumbar fusion
The spinopelvic relationship plays a crucial role in determining the extent of correction required in lumbar spinal fusion surgeries to restore proper alignment for a patient. This intricate interplay between the spine and pelvis significantly influences surgical planning and decision making to achieve optimal outcomes. Traditionally, reconstructive spine surgery has focused on sagittal alignment and coronal alignment, as they are heavily correlated with health-related quality of life scores, including Oswestry Disability Index (ODI) (35).
Recent studies have further explored spinopelvic parameters in relation to patient outcomes after lumbar fusion. Specifically, larger PI, SS, and PI-LL mismatch were found to be associated with increased hip joint narrowing, particularly in non-arthritic hips and after long spinal fusion procedures (36). This observation suggests that greater PI and SS values may lead to increased transmission of forces to the spine and pelvis, resulting in heightened hip joint narrowing post-fusion. Surprisingly, no significant association was found between PT, SVA, and LL hip joint narrowing rate, despite LL’s correlation with PI. These findings highlight the complexities involved in optimizing PI-LL, especially when dealing with larger PI values, and underscore the importance of achieving appropriate correction to mitigate the risk of hip joint narrowing after spinal fusion procedures (36). One limitation of this study would be no control for spinal fusion indication, meaning some patients may have had diagnoses that may be prone to developing joint degeneration. Another study focused on patients with severe adolescent idiopathic scoliosis who underwent spinal fusion, analyzing their long-term outcomes after a minimum of 40 years of follow-up (37). Their findings showed that SVA values exceeding 5 cm were associated with poorer functional outcomes, while PT exhibited no significant correlation with function. Unsurprisingly, achieving a PI-LL mismatch of ≤9° was strongly linked to improved function during long-term follow-up, showcasing higher quality-of-life scores (37). One major limitation of this study is the absence of lateral radiographs at the time of posterior spinal fusion, which did not allow for assessment of change in LL through the follow-up period. These studies emphasize the impact of a patient’s preexisting spinal pathology on operative planning and highlight the parameters that should be considered prior to surgery.
A recent study explored the impact of previous spine fusion on symptoms related to limb length discrepancy in patients with THA. They found that in patients who underwent both THA and spinal fusion, the occurrence of perceived limb length discrepancy, limping, and aggravated back pain after THA was higher compared to patients without fusion. These differences were observed even in patients with leg-length discrepancy typically considered to be subclinical (i.e., ≤10 mm), suggesting particular care should be taken to ensure minimization of any potential limb length discrepancy in patients with previous spinal fusion (38).
Updates on spinopelvic parameters and their utility
Emerging data suggests that additional spinopelvic parameters should be considered to mitigate the risk of dislocations and complications following THA. The combined sagittal index (CSI) is a parameter recently introduced by Heckmann et al. to assess sagittal, functional hip motion (13). It aims to expand the conventional safe zone for acetabular implantation, which was previously based on the coronal plane, to a new safe zone based on the sagittal plane. The CSI is calculated by combining the acetabular AI angle and the pelvic femoral angle (PFA). The PFA indicates the sagittal position of the femur and its movement relative to the pelvis, with average values of 180° in a standing position and 125° in a sitting position. The AI reflects the sagittal orientation of the acetabular component and is influenced by anteversion and inclination (10,13). Deviations from normal CSI values are associated with an increased risk of impingement and dislocation.
When the pelvis shifts, such as in cases of anterior or posterior tilt, the SS adapts accordingly. In spinopelvic parameters, this is seen as an increase in posterior PT with an accompanied equivalent decrease in SS, which is a necessity to keep PI constant. This reduction in SS also often results in a reduction in LL. As highlighted by Roussouly and colleagues, a patient’s distinct PI impacts multiple aspects of their spinal morphology including LL. A loss of LL due to spondylosis or prior surgery may result in a PI-LL mismatch that significantly influences a patient’s global sagittal balance, a parameter that has become increasingly common (12). Luthringer et al. defines a normal LL as PI-LL ±10° (39). When the PI-LL difference is >10°, it is considered a mismatch and indicates a flatback deformity (posterior PT). Each additional degree of increased posterior PT results in an increase in functional acetabular anteversion of 0.7° (40). To ensure precision, the reference plane during surgery should be based on the standing anterior posterior (AP) pelvis, or the “functional pelvic plane” (39).
Spinal mobility is also important to consider and can be categorized into three types based on the difference in SS (ΔSS) between standing and sitting: normal (10°–30°), hypermobile (>30°), and stiff (<10°) (41). Despite current emphasis on ΔSS as a surrogate for spinal stiffness, a recent study demonstrates that ΔSS may be a poor independent predictor of spinopelvic mobility (42). Instead, the change in LL between sitting and standing (ΔLL) has been proposed as a more accurate measure of spine mobility. Given its ability to better assess spinopelvic motion in stiff patients, ΔLL is recommended as the appropriate metric to evaluate spinal motion in patients with lumbar pathology.
A recent 2023 study by Mills et al. sought to further explore the relationship between ΔSS and ΔLL, while providing a more comprehensive assessment of how these metrics capture spinal mobility (43). The authors found that 20% of patients classified as having a normal or hypermobile spine by ΔSS were found to have stiff spines when classified by ΔLL. This discrepancy emphasizes the importance and utility of ΔLL as a viable parameter for spinopelvic mobility and risk assessment in THA, in addition to highlighting a group of patients that may have a higher dislocation risk not appreciated when evaluated on ΔSS alone.
Strengths and limitations
The strengths of this review include the complete review of recent literature on spinopelvic parameters and their impact on THA and spine fusion, presentation of novel spinopelvic parameters, and discussion of how these novel parameters may influence future surgical management. The limitation of this review is that it is not a systematic review, and thus does not include every article published on the topic. Further, given the heterogeneity in the number of spine levels fused and the differences in whether the spine surgery was performed before or after the hip arthroplasty, a meta-analysis on the topic would not be methodologically prudent. Additional, data is needed to further define how to obtain optimal outcomes and which patients should have hip or spine surgery first. However, we present a pragmatic review of parameters that should be considered in routine management of patients with hip and spine pathology.
Conclusions
The lumbar spine, pelvis, and hips work together to maintain appropriate posture, balance, and function in healthy patients. When one of these elements begins to break down, compensatory mechanisms may lead to abnormal alignment. As a result, spine pathology can present with subsequent hip pain and can cause low back pain. Traditional parameters that have been used to assess the functional relationship of these structures continue to be of use in evaluating and managing patients with spine and hip pathology. New interpretations and applications of these parameters may decrease risk, prevent complications, and improve outcomes for patients who experience these associated, and often concurrent, pathologies. Given the lack of concrete data on the topic, a reasonable approach may be to perform hip arthroplasty prior to a multilevel spinal fusion, especially when the fusion includes the pelvis. However, for patients with radiculopathy requiring a simpler one- or two-level spinal fusion, the spine may be safely addressed first to relieve the patient of radiculopathy prior to proceeding with a hip arthroplasty. Future reviews highlighting the relationship between lumbar disc arthroplasty (LDA) and hip parameters, including potential timing of LDA and THA, would be an insightful addition to this review.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, AME Medical Journal for the series “Degenerative Spine Disease”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://amj.amegroups.com/article/view/10.21037/amj-23-163/rc
Peer Review File: Available at https://amj.amegroups.com/article/view/10.21037/amj-23-163/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj-23-163/coif). The series “Degenerative Spine Disease” was commissioned by the editorial office without any funding or sponsorship. M.J.L. served as the unpaid Guest Editor of the series. A.R.V. received royalties from Aesculap, Atlas Spine, Clobus, Medtronic, SpineWave, Stryker, Elsevier, Jaypee, Taylor Francis, Thieme and Support for attending meetings and from AO Spine. He holds stocks in the Advanced Spinal Intellectual Properties, Atlaas Spine, Avaz Surgical, Bonovo, Computational Dynamics, Cytonics, Dep Health, Dimension Orthotics, Electrocore, Flagship Surgical, FlowPharma, Globus, Innovative Surgical Design, Insight Therapeutics, Jushi, Orthobullets, Nuvasive, Orthobullets, Paradigm Spine, Parvizi Surgical, Progressive Spinal Technologies, Replication Medica, Spine Medica, Spinology, Stout Medical, Vertiflex, ViewFi Health. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rivière C, Lazennec JY, Van Der Straeten C, et al. The influence of spine-hip relations on total hip replacement: A systematic review. Orthop Traumatol Surg Res 2017;103:559-68. [Crossref] [PubMed]
- Devin CJ, McCullough KA, Morris BJ, et al. Hip-spine syndrome. J Am Acad Orthop Surg 2012;20:434-42. [Crossref] [PubMed]
- Chavarria JC, Douleh DG, York PJ. The Hip-Spine Challenge. J Bone Joint Surg Am 2021;103:1852-60. [Crossref] [PubMed]
- Hasegawa K, Dubousset JF. Cone of Economy with the Chain of Balance-Historical Perspective and Proof of Concept. Spine Surg Relat Res 2022;6:337-49. [Crossref] [PubMed]
- Ames CP, Smith JS, Scheer JK, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults: A review. J Neurosurg Spine 2012;16:547-64. [Crossref] [PubMed]
- Roussouly P, Pinheiro-Franco JL. Sagittal parameters of the spine: biomechanical approach. Eur Spine J 2011;20:578-85. [Crossref] [PubMed]
- Hawes MC, O’brien JP. The transformation of spinal curvature into spinal deformity: pathological processes and implications for treatment. Scoliosis 2006;1:3. [Crossref] [PubMed]
- Celestre PC, Dimar JR 2nd, Glassman SD. Spinopelvic Parameters: Lumbar Lordosis, Pelvic Incidence, Pelvic Tilt, and Sacral Slope: What Does a Spine Surgeon Need to Know to Plan a Lumbar Deformity Correction? Neurosurg Clin N Am 2018;29:323-9. [Crossref] [PubMed]
- Batra S, Khare T, Kabra AP, et al. Hip-spine relationship in total hip arthroplasty – Simplifying the concepts. J Clin Orthop Trauma 2022;29:101877. [Crossref] [PubMed]
- Mancino F, Cacciola G, Di Matteo V, et al. Surgical implications of the hip-spine relationship in total hip arthroplasty. Orthop Rev (Pavia) 2020;12:8656. [Crossref] [PubMed]
- Pizones J, García-Rey E. Pelvic motion the key to understanding spine-hip interaction. EFORT Open Rev 2020;5:522-33. [Crossref] [PubMed]
- Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 2011;20:609-18. [Crossref] [PubMed]
- Heckmann N, McKnight B, Stefl M, et al. Late Dislocation Following Total Hip Arthroplasty: Spinopelvic Imbalance as a Causative Factor. J Bone Joint Surg Am 2018;100:1845-53. [Crossref] [PubMed]
- Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 2001;10:314-9. [Crossref] [PubMed]
- Le Huec JC, Faundez A, Dominguez D, et al. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop 2015;39:87-95. [Crossref] [PubMed]
- Malkani AL, Garber AT, Ong KL, et al. Total Hip Arthroplasty in Patients With Previous Lumbar Fusion Surgery: Are There More Dislocations and Revisions? J Arthroplasty 2018;33:1189-93. [Crossref] [PubMed]
- Sing DC, Barry JJ, Aguilar TU, et al. Prior Lumbar Spinal Arthrodesis Increases Risk of Prosthetic-Related Complication in Total Hip Arthroplasty. J Arthroplasty 2016;31:227-232.e1. [Crossref] [PubMed]
- Lazennec JY, Clark IC, Folinais D, et al. What is the Impact of a Spinal Fusion on Acetabular Implant Orientation in Functional Standing and Sitting Positions? J Arthroplasty 2017;32:3184-90. [Crossref] [PubMed]
- Bernstein J, Charette R, Sloan M, et al. Spinal Fusion Is Associated With Changes in Acetabular Orientation and Reductions in Pelvic Mobility. Clin Orthop Relat Res 2019;477:324-30. [Crossref] [PubMed]
- Kawai T, Shimizu T, Goto K, et al. Number of Levels of Spinal Fusion Associated with the Rate of Joint-Space Narrowing in the Hip. J Bone Joint Surg Am 2021;103:953-60. [Crossref] [PubMed]
- Ukai T, Katoh H, Yokoyama K, et al. Effect of spinal fusion on joint space narrowing of the hip: comparison among non-fusion, short fusion, and middle or long fusion. J Orthop Traumatol 2023;24:1. [Crossref] [PubMed]
- Kim Y, Vergari C, Shimizu Y, et al. The Impact of Hip Mobility on Lumbar and Pelvic Mobility before and after Total Hip Arthroplasty. J Clin Med 2022;12:331. [Crossref] [PubMed]
- Gausden EB, Parhar HS, Popper JE, et al. Risk Factors for Early Dislocation Following Primary Elective Total Hip Arthroplasty. J Arthroplasty 2018;33:1567-1571.e2. [Crossref] [PubMed]
- Rainer WG, Abdel MP, Freedman BA, et al. Pelvic Tilt and the Pubic Symphysis to Sacrococcygeal Junction Distance: Risk Factors for Hip Dislocation Observed on Anteroposterior Pelvis Radiographs. J Arthroplasty 2021;36:S367-73. [Crossref] [PubMed]
- An VVG, Phan K, Sivakumar BS, et al. Prior Lumbar Spinal Fusion is Associated With an Increased Risk of Dislocation and Revision in Total Hip Arthroplasty: A Meta-Analysis. J Arthroplasty 2018;33:297-300. [Crossref] [PubMed]
- Bala A, Chona DV, Amanatullah DF, et al. Timing of Lumbar Spinal Fusion Affects Total Hip Arthroplasty Outcomes. J Am Acad Orthop Surg Glob Res Rev 2019;3:e00133. [Crossref] [PubMed]
- Malkani AL, Himschoot KJ, Ong KL, et al. Does Timing of Primary Total Hip Arthroplasty Prior to or After Lumbar Spine Fusion Have an Effect on Dislocation and Revision Rates? J Arthroplasty 2019;34:907-11. [Crossref] [PubMed]
- Yang DS, Li NY, Mariorenzi MC, et al. Surgical Treatment of Patients With Dual Hip and Spinal Degenerative Disease: Effect of Surgical Sequence of Spinal Fusion and Total Hip Arthroplasty on Postoperative Complications. Spine (Phila Pa 1976) 2020;45:E587-93. [Crossref] [PubMed]
- Goyal DKC, Divi SN, Vaccaro AR, et al. Stability in Direct Lateral vs Direct Anterior Total Hip Arthroplasty in the Context of Lumbar Spinal Fusion. J Am Acad Orthop Surg 2022;30:e628-39. [Crossref] [PubMed]
- Kahn TL, Kellam PJ, Anderson LA, et al. Can Dislocation Rates Be Decreased Using the Anterior Approach in Patients With Lumbar Spondylosis or Lumbar Instrumented Fusion? J Arthroplasty 2021;36:217-21. [Crossref] [PubMed]
- Minutillo GT, Woo D, Granruth CB, et al. Prosthetic Hip Dislocations in Direct Anterior Versus Posterior Approach in Patients With Instrumented Lumbar Fusion. J Arthroplasty 2023;38:S95-S100. [Crossref] [PubMed]
- Sultan AA, Khlopas A, Piuzzi NS, et al. The Impact of Spino-Pelvic Alignment on Total Hip Arthroplasty Outcomes: A Critical Analysis of Current Evidence. J Arthroplasty 2018;33:1606-16. [Crossref] [PubMed]
- Phan D, Bederman SS, Schwarzkopf R. The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J 2015;97-B:1017-23. [Crossref] [PubMed]
- Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 1978;60:217-20. [Crossref] [PubMed]
- Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682-8. [Crossref] [PubMed]
- Kawai T, Shimizu T, Goto K, et al. The Impact of Spinopelvic Parameters on Hip Degeneration After Spinal Fusion. Spine (Phila Pa 1976) 2022;47:1093-102. [Crossref] [PubMed]
- Rubery PT, Lander ST, Mesfin A, et al. Mismatch Between Pelvic Incidence and Lumbar Lordosis is the Key Sagittal Plane Determinant of Patient Outcome at Minimum 40 Years After Instrumented Fusion for Adolescent Idiopathic Scoliosis. Spine (Phila Pa 1976) 2022;47:E169-76. [Crossref] [PubMed]
- Pheasant MS, Coulter JL, Wallace C, et al. Lumbar Spine Fusion and Symptoms of Leg Length Discrepancy After Hip Arthroplasty. J Arthroplasty 2021;36:3241-3247.e1. [Crossref] [PubMed]
- Luthringer TA, Vigdorchik JM. A Preoperative Workup of a “Hip-Spine” Total Hip Arthroplasty Patient: A Simplified Approach to a Complex Problem. J Arthroplasty 2019;34:S57-70. [Crossref] [PubMed]
- Lembeck B, Mueller O, Reize P, et al. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop 2005;76:517-23. [Crossref] [PubMed]
- Stefl M, Lundergan W, Heckmann N, et al. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J 2017;99-B:37-45. [Crossref] [PubMed]
- Sharma AK, Grammatopoulos G, Pierrepont JW, et al. Sacral Slope Change From Standing to Relaxed-Seated Grossly Overpredicts the Presence of a Stiff Spine. J Arthroplasty 2023;38:713-718.e1. [Crossref] [PubMed]
- Mills ES, Wang JC, Sanchez J, et al. The Correlation Between Pelvic Motion and Lumbar Motion in Patients Presenting With a Lumbar Spinal Pathology: Implications for Assessing Dislocation Risk in Total Hip Arthroplasty. Arthroplast Today 2023;20:101105. [Crossref] [PubMed]
Cite this article as: McCurdy M, Lee Y, DiNicola G, Ku A, Vaccaro AR, Hilibrand AS, Schroeder GD, Kepler CK, Lambrechts MJ. The hip spine relationship—what we know and what we don’t: a narrative review. AME Med J 2024;9:6.