
A narrative review of treatment of the elderly patient: do we need to alter surgical management of lumbar spine disease?
Introduction
Background
The global population is aging, with an upward demographic shift that is rapidly expanding the elderly. In the United States, the proportion of the elderly defined as 65 years old and older is expected to double from 2015 to 2050, with the “super-elderly”, aged at least 80 years old and older expected to more than triple over the same period (1). This demographic shift signals an increasing burden of degenerative pathology, and degenerative lumbar conditions including symptomatic stenosis, spondylolisthesis, and associated deformity (2). Lumbar stenosis remains the most common indication for spine surgery for elderly patients, and rates of complex surgeries including long fusions and instrumented fusions are also increasing (3). While surgery can be considered for these conditions with failure of appropriate nonsurgical management, the elderly population presents a unique challenge.
Rationale and knowledge gap
Age is often associated with frailty, increased comorbidities, diminished functional capacity and consequently tempered expectations with surgery. Indeed, lumbar pathology in particular can limit function and activity while requiring increased healthcare resources with age, impacting even mortality (4). Elderly patients, their family practitioners, and surgeons often expect that they will have more complications or greater loss of independence following surgical management that impedes any benefit from surgery. Concern persists particularly in the lay press about the safety and efficacy of spine surgery in elderly patients (5-7). However, many of these patients and their families have limited information to weigh the relevant risks and benefits. In addition, expectations of function late in life and life expectancy itself continue to change. The elderly have enjoyed increased quality of life later in life. Greater expectations for activity and function influences approaches to healthcare and utilization of surgery. Furthermore, while average life expectancy for a woman in the United States remains close to 80 years, average life expectancy for women at age 80 is 9.1 years (8). As patients anticipate active lifestyles at age 65, 75, and 85, how will realistic surgical goals for these patients change?
Surgeons responding to these changes have sought to reduce the invasiveness and physiologic impact of spine surgery to limit harm. This raises questions of when and how surgical management for the elderly should be altered to limit risk of complication while still achieving goals of improved pain and function. For example, the role of fusion in the setting of stenosis with stable degenerative spondylolisthesis as well as the benefits of certain instrumentation or interbodies for fixation in fusion remain in question (9,10). This supports a cautious approach to a population with lower functional demand. Outcomes of surgery could be limited, however, if instability or persistent neurologic compression are not addressed to reduce invasiveness.
Objective
Both patients and providers must understand the risks and outcomes of spine surgery for lumbar pathology in the elderly population to allow for appropriate, informed, and shared decision-making. While safe and effective surgery remains challenging in some patients, the coming demographic shift and increased expectations will make it increasingly important to address lumbar spine pathology pragmatically. This review is focused on comorbidities and frailty in elderly patients undergoing lumbar spine surgery, the risks and outcomes of lumbar spine surgery in elderly patients, and the techniques and protocols available to reduce surgical risk and variability while achieving similar surgical goals. I present this article in accordance with the Narrative Review reporting checklist (available at https://amj.amegroups.com/article/view/10.21037/amj-23-150/rc).
Methods
A narrative review of lumbar spine surgery in elderly populations was completed. This included a search of the MEDLINE database through May 2023 (Table 1). The search was limited to human studies published in the English language. This generated 69 results, with case series of over 10 patients, cohorts, or controlled trials reviewed with their relevant references. Studies were evaluated for the impact on the article topic. Elderly was defined by age ≥65 similar to U.S. Census Bureau and World Health Organization definitions (1). Super-elderly includes a much older subset of the elderly and varies in the literature from 80–90 years of age or older. For this review, a broader definition of super-elderly age ≥80 was used to include the available spine literature using this term.
Table 1
| Items | Specification |
|---|---|
| Date of search | May 25th, 2023 |
| Databases and other sources searched | MEDLINE |
| Search terms used | “Lumbar spine surgery” AND (“elderly” OR “geriatric”) AND (“outcomes” OR “complications” OR “fusion”) |
| Timeframe | Through May, 2023 |
| Inclusion criteria | English language studies including case series, cohorts, or controlled trials |
| Selection process | Assessment for impact on article topic |
Three representative cases were generated with deidentified data in compliance with institutional review board approval.
Lumbar surgery in the elderly
Comorbidities in the elderly
Age is associated with increased rates of comorbidities as chronic and degenerative diseases progress (11). Elderly patients aged 65 and older have on average at least one medical comorbidity requiring chronic treatment and 50% have two (12). Moreover, age is also associated with the degenerative cascade in the lumbar spine (13). Other pathologies that impact the lumbar spine and its treatment including osteoporosis and sarcopenia also increase in frequency with age. Age therefore is associated with both increased rates of symptomatic lumbar pathology while increasing medical complexity and risk.
Several systems have been developed to assess patient comorbidities and their impact on perioperative risk and outcomes. The American Society of Anesthesiologists (ASA) physical status classification broadly categorizes patients by their qualitative and relative morbidity from normal health to severe systemic disease, moribund patients not expected to survive, and brain-dead patients undergoing donor organ recovery (14). Other systems can provide more detailed evaluation and may provide a more comprehensive evaluation of the burden of comorbidity. The Charleston Comorbidity Index (CCI) was developed to evaluate comorbidities effect on 10-year mortality (14). It has been used frequently in the spine literature to identify predictors of surgical complications. In one study of 226 lumbar surgeries, ASA and CCI were significantly correlated with one another (Spearman ρ=0.458, P<0.001), as well as age (P<0.0001) (14). Increasing CCI was associated with increasing likelihood of any complication (P=0.0093) and minor complication (P=0.0032). Increasing ASA grade was associated with increasing likelihood of a major complication (P=0.0035). Other studies have supported these results, although neither ASA or CCI can completely explain complication occurrence (15).
Other measures of patient frailty have been developed that include both patient comorbidities and function. Such frailty indices have similarly been utilized to assess patient’s expected risk of complication following lumbar spine surgery and have been associated with perioperative morbidity and mortality (16). Simple 5- or 11-item indices (mFI-5 and mFI-11) including categorical measures of independent functional status and other comorbidities have been used frequently to assess perioperative risk in spine surgery. In both elderly and super-elderly populations, the mFI-11 has been associated with complications as well as mortality (17,18). This system of evaluation has limitations, however. Many existing studies, including the ones above, include few patients with severe frailty. Others found conflicting results, with no association between the mFI-5 or mFI-11 and complications or mortality in the elderly undergoing lumbar spine surgery (19).
The association of age with comorbidities and the consequently increased risk of surgical complications associated with these comorbidities raises surgical risk in the elderly. These factors should be identified and, when possible, addressed before surgery (20).
Nonsurgical care
Given the elevated risks of surgical complications in older age, appropriate nonsurgical care should be considered before elective lumbar spine surgery. Lumbar surgery is indicated prior to nonsurgical management for patients with severe or progressive neurologic deficits. However, extensive nonsurgical management is reasonable when surgical risk is significantly elevated for elective degenerative lumbar pathology. Nonsurgical treatment can vary, including activity modifications, physical therapy, medications, and injections (21). Many alternatives are available to patients, including acupuncture, massage, transcutaneous electrical nerve stimulation, and chiropractic; there is limited evidence however for these modalities and some are associated with risk with spinal pathology.
These options may provide clinical benefit for the elderly similar to younger populations. Good or excellent outcomes can be obtained with nonsurgical management in elderly patients; however, outcomes may remain poor for those who fail to improve. For example, in a prospective study of patients aged >70 undergoing nonsurgical treatment versus surgery for lumbar stenosis with 10-year follow-up, nonsurgical treatment was associated with decreased clinical improvement and satisfaction (21). Indeed, other studies have found older age predictive of a poorer outcome with nonsurgical management (22). However, larger studies evaluating nonsurgical care specifically in the elderly population have been limited.
Pain and functional limitations due to lumbar spinal pathology can be successfully managed with nonsurgical care in the elderly, similar to other age groups. However, nonsurgical management may fail for some elderly patients and may provide poorer outcomes and satisfaction versus surgical treatment when indicated. Therefore, careful consideration of surgery may be necessary when appropriate nonsurgical management has failed.
Efficacy and safety of surgical care
Risk and outcomes
The efficacy and safety of surgery in elderly patients has been questioned due to the association of older age with comorbidities and complications. Nonsurgical options may not meet the expectations of elderly patients who have persistent pain or loss of function, and surgical options may be considered. There is an increasing body of literature evaluating the outcomes and surgical risk for lumbar pathology in elderly patients. We have evaluated these studies to determine whether lumbar spine surgery can provide clinical improvement in elderly relative to younger patients without unacceptable rates of complications. It is also important to understand whether even older patients, such as the previously defined super-elderly age 80 or older, may be at greater risk with surgery or no longer benefit from surgical intervention. Finally, the evidence evaluating surgical invasiveness and relative impact of fusion and instrumentation on outcomes in the elderly population was reviewed.
Earlier studies identified age as a strong risk factor for complications following lumbar surgery. These studies have raised persistent concern for surgery for elderly patients. Deyo et al. evaluated the impact of age on complication rates following lumbar decompression as well as lumbar decompression and fusion for degenerative lumbar pathology utilizing Washington State registry data from the Commission Hospital Abstract Reporting System from 1986–1988 (23). This registry included only data from hospitalizations. Complication rates consistently increased with age, with patients aged ≥75 almost 3 times more likely to have a complication than those under 40 years old (17.7% versus 6.4%). They reported a relative risk (RR) of 4.20 [95% confidence interval (CI): 0.05–0.75] per 10-year increment in age. Complications were more common with fusion (17.4%) than decompression alone (7.6%, RR =2.00). Complication severity was not reported in detail; however, length of stay, hospital charges, and mortality were all higher in the group age ≥75 as well. The authors suggested that mortality and other complication rates were not “prohibitive” to surgery in even the oldest patients. Clearly however increased risk should be considered when surgery is offered in this population. Carreon et al. later evaluated 98 patients aged ≥65 undergoing lumbar fusion and found that complications correlated with older age in addition to operative time, blood loss and number of fusion levels (24). The authors reported an overall compilation rate of 80%, with 21.4% of patients experiencing a major complication. Despite these high rates, the authors suggested that surgery could be considered in the elderly population. These studies did rigorously assess patient comorbidities and other factors associated with age nor how patients were optimized for surgery. They did however paint a clear picture of surgical risk in the elderly population. Their results provided evidence of risk in surgical management with age, giving credence to the concerns for elderly patients both by surgeons and in the lay press. Since that time however, conflicting studies have reported varying complication rates by age for lumbar surgeries with risks for elderly patients often matching younger populations.
Glassman et al. evaluated 97 consecutive patients over age 65 who underwent lumbar decompression and fusion for degenerative pathology (25). Health-related quality of life scores improved for all patients except general health, and that with only a small decline. Outcomes were not associated with complications. Acosta et al. evaluated 73 patients who underwent multilevel anterior lumbar interbody fusion (ALIF) with posterolateral lumbar fusion with instrumentation for symptomatic lumbar degenerative disc disease (26). Thirty patients were at least 65 years old, and 43 patients were younger. Mean follow-up was 19 months. There were no significant differences in perioperative complications between the groups. There were no statistically significant differences in the improvement in back pain or in the rates of fusion between the groups at last follow-up. Clinical outcomes in the elderly were comparable to those of younger patients. Okuda et al. evaluated an elderly (mean age 74 years) cohort of 31 patients in comparison with a younger (mean age 59 years) cohort of 70 patients who underwent posterior lumbar interbody fusions (PLIFs). There were no differences in outcome by age; however, subsidence and delayed union were more common in the elderly (27). The fusion results did not impact clinical outcomes in this study.
These studies have limitations. Most have a small sample size that limits their power to identify differences in outcome associated with age. Comparisons and analysis of specific complications more common in the elderly were limited. Retrospective studies evaluating the association of age with surgical complications will also be strongly influenced by selection bias. Elderly patients without appropriate optimization would be unlikely to be included. Therefore, differences in safety and efficacy by age may be small or not determinable. In a systematic review by Cloyd et al. that included 27 articles evaluating lumbar spine surgery in elderly patients, most of the included studies were retrospective cohorts or clinical case series with similar limitations (28). These studies are difficult to compare as they rarely include similar interventions indicated for a similar population of patients. The review reported widely varying complication rates following decompression for lumbar stenosis in elderly patients age ≥65 from 2.5–80%. Despite these limitations, age is a clear risk factor for complications in many studies. However, it is also clear that this association can be moderated by optimization and appropriate patient selection. In such groups of elderly patients, complication rates and patient reported outcomes remain similar to younger patients.
Risk and outcomes in the super-elderly
As comorbidity and surgical risk may both increase with age, investigators have questioned whether the super-elderly over age 80 are at higher risk than their younger elderly counterparts. Several studies have confirmed increased risk in this even older population. For example, Raffo and Lauerman found that 20 patients ≥80 years with lumbar stenosis undergoing lumbar fusion had a 35% major complication rate (29), much higher than rates in similar studies of younger elderly patients (23,24). Comorbidities, length of stay, and the need for intensive care unit monitoring were the only factors associated with this high rate of complication, emphasizing the need for evaluation of health and frailty in this population.
Outcomes have varied in other studies. Wang et al. evaluated 26 patients over age 85 undergoing lumbar decompressive or fusion surgery with a minimum 24 months of follow-up (30). The authors reported a complication rate of 19.2% (2 major and 3 minor). While they also found no association of age even >90 with complication, the study was not powered for this outcome. Operative time over 180 minutes was associated with complication (P=0.0134). The authors concluded that lumbar spine surgery could be safely accomplished in super-elderly patients. Son et al. evaluated a cohort of 30 patients age ≥80 years (mean 82.0 years) in comparison to 130 patients age 65–80 years (mean 71.6 years) undergoing elective lumbar fusion for degenerative stenosis (31). Over 1 year of follow-up, both groups had similar improvement in pain and function scores, with no differences in overall early or late complications. The ≥80 years group had only a higher rate of postoperative delirium. Gerhardt et al. evaluated 244 patients (mean age 83.1±3 years) who underwent decompression for stenosis or disc herniation (32). The overall surgical complication rate was 22.5%, with a mortality rate of 0.8%. Despite these complications, the authors suggested that lumbar spine surgery was acceptable for even super-elderly patients.
Similarly high complication rates can be found in well selected super-elderly patients, even if outcomes remain improved. For example, Balabaud et al. evaluated 121 consecutive patients aged ≥80 years (mean 83.2±2.4 years) undergoing lumbar decompression with or without fusion for lumbar degenerative pathology (33). Major complications occurred in 13% of patients; however, there were no recorded deaths at 1-year follow-up (average follow-up 24.3±16.5 months). Blood loss, operative time, instrumentation, previous surgery and dural tears were associated with rates of complications. Bouloussa et al. evaluated 49 patients over age 85 (mean age 87.5, follow-up 27.4 months) who underwent decompression with or without fusion for lumbar degenerative stenosis (34). Minor complications were frequent (38.7%), and major complications were not uncommon (12.2%). The perioperative mortality rate was 0.2%. Despite this high rate of complications, although more frequently minor, 41 patients were very satisfied (83.7%) and five patients were satisfied (10.2%). Liu et al. found a complication rate of 15.3% in a super-elderly cohort of 202 patients (age range 77–92 years) undergoing lumbar fusion (35). Major complications were associated with age [odds ratio (OR): 1.323, 95% CI: 1.126–1.554], and were 10-fold higher in patients over age 80 versus younger patients. Saleh et al. evaluated the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) Database for minor and major complications, mortality, and readmissions in geriatric patients over age 80 who underwent lumbar spinal surgery in the decade from 2005–2015 (36). This included 2,320 patients with an overall complication rate of 16.34%. Major complications occurred at a rate of 3.23%, with a mortality rate of 0.43%. Notably, increased operative time (>180 minutes, OR: 3.07, 95% CI: 2.23–4.22) and use of instrumentation and fusion (OR: 2.56, 95% CI: 1.66–3.94) were associated with complications.
Arinzon et al. evaluated geriatric patients age 65–74 (n=179) versus ≥75 (n=104) (37). Within both treatment groups, there was a significant (P<0.0001) subjective improvement in low back and radicular pain, as well as the ability to perform daily activities. When compared to preoperative levels, pain while performing daily activities were significantly improved in both treatment groups (P<0.001). The overall postoperative complication rate was similar between the groups; however, elderly patients with diabetes did have reduced benefit from surgery with nearly double the complication rate. Notably, patients aged over 80 years had greater relative improvement in symptoms after surgery than younger patients. Rault et al. also found no increase in major complications in patients over age 80 (38). Minor complications were however more frequent in older patients. Cardiac history, prior laminectomy, age-adjusted CCI and incidental durotomy were independent risk factors for major complications. Rihn et al. evaluated 105 patients aged ≥80 with stenosis and degenerative spondylolisthesis from the Spine Patient Outcomes Research Trial (39). These patients were compared to 1,130 younger patients in the trial. Older patients had a higher disease burden with higher rates of multilevel stenosis, severe stenosis, and asymmetric motor weakness, as well as a higher medical comorbidity burden with higher rates of cardiac disease and osteoporosis. Of the super-elderly patients, 58 underwent surgery. There were no differences in postoperative complications or reoperations between these patients and those under age 80. Mortality was also similar in the super-elderly group. The benefits of surgery were significant and similar to younger patients excepting for the SF-36 bodily pain domain and self-rated major improvement, both of which were improved but with a smaller treatment effect.
Poorer outcomes have also been published for super-elderly patients. Tan et al. evaluated 47 patients aged ≥80 who underwent a variety of surgeries for indications that varied from degeneration to trauma and infection (40). This cohort had many comorbidities with ≥3 in 34%. They found mortality rates of 2.1% in the first 30 days, and 12.8% in the following 2 years. Patients with multiple comorbidities and nondegenerative etiologies had higher mortality rates, suggesting a more medically complex and nonelective population. These outcomes are not generalizable to the optimized elderly patient, however indicate that surgical intervention for the super-elderly with multiple or severe complications has far higher perioperative risk. Patients with such comorbidities should be informed about high surgical risks even if considered urgent or nonelective.
Larger data studies remain helpful to provide a broader perspective on surgical complications in the super-elderly. Lagman et al. analyzed 10,232 elderly patients (age ≥80) out of 155,720 total patients undergoing decompression without fusion, fusion without decompression, or decompression with fusion in the MarketScan database from 2000–2012 (41). This database includes inpatient and outpatient encounters, although is limited to the duration of a patient’s insurance enrollment. Older patients had higher rates of length of stay (3.62 versus 3.11 days; P<0.0001), in hospital mortality (0.31% versus 0.06%; P<0.0001), as well as 30-day complication rates (17.8% versus 12.6%; P<0.0001). McGirt et al. utilized the National Neurosurgery Quality and Outcomes Database registry, including outcome and complication data up to 1 year, to evaluate the efficacy, morbidity other outcomes of surgical management of degenerative lumbar pathology in patients age ≥70 versus younger patients (42). They evaluated 4,370 patients, of whom 1,020 were ≥70 years. The elderly patients had higher rates of comorbidities including cardiac disease, osteoporosis, and had higher ASA classes. Elderly patients had surgeries involving 3 or more levels more frequently; however, there were similar rates of arthrodesis (38% in each group). Length of stay was greater in the elderly population; however, complication and readmission rates were similar. Moreover, both elderly and non-elderly patients had clinically significant and equivalent improvements in pain, function and other patient reported outcome measures.
The above studies have significant limitations with alternatively small sample size, heterogeneous populations and procedures, or selection biases. However, most suggest that lumbar spinal surgery results in significant improvement in pain, disability, and quality of life of patients of any age. Both elderly and super-elderly patients found significant benefits with high rates of satisfaction. Several studies found that surgical benefits did not invariably come the cost of more dramatically increased rates of surgical complications. In the super-elderly however, comorbidities and other risk factors including CCI, ASA, and perioperative factors including surgical duration, blood loss, and intensive care unit utilization were associated with higher rates of postoperative complications including mortality. While these data justify the cautious but continued use of lumbar surgery for well selected and optimized elderly patients, super-elderly patients should be informed regarding their risk relative to younger patients. This is particularly relevant improving functional demands in this population.
Surgical invasiveness
The desire to reduce the physiologic burden of surgery for elderly patients had raised interest in avoiding larger, longer, more complex and bloodier surgeries. As suggested in the above studies, fusion in general and longer fusions may be risk factors for complications (23). For more common pathologies, such as lumbar stenosis with relatively stable spondylolisthesis, both decompression and decompression with fusion may offer benefit and therefore decompression alone is often recommended for elderly patients. The relative benefit however of a more limited surgical episode however remains unclear, particularly as there is a potential harm to withholding otherwise indicated management of structural pathology, instability, residual stenosis including vertical foraminal stenosis, or other factors that influence outcome.
Few studies directly compare decompression alone to decompression with fusion, and significant spondylolistheses or instability were frequently excluded. Lee et al. evaluated 25 patients undergoing a PLIF for lumbar stenosis without spondylolisthesis over 5 mm, matched to 25 patients undergoing decompression alone with minimum 2-year follow-up (43). Patients were revised in the decompression group at twice the rate versus the fusion group (16% versus 8%). Back pain scores improved to a greater extent also in the fusion versus decompression group (P<0.01). Ragab et al. evaluated 118 patients aged ≥70 with lumbar stenosis with or without stable spondylolisthesis with an average 7 years of follow-up (44). In this group, 38% underwent a fusion procedure. Outcomes were improved with high satisfaction regardless of procedure. Based on a qualitative evaluation of back and leg pain, activity and medication requirements, patients who underwent decompression alone had similar good or excellent outcomes (93.1%) to patients who underwent decompression and fusion (91.1%).
Other studies evaluated the outcomes of instrumented fusion in older versus younger patients. Between elderly and nonelderly patients, there were no differences in complication rates with PLIF with posterior fusion and pedicle screw instrumentation (28,43,45,46), transforaminal lumbar interbody fusion (47,48), ALIF (27), and posterior decompression and fusion with pedicle screw instrumentation (49-51). Notably, pseudarthrosis and use of interbodies did not impact clinical outcomes in some studies in this population, although not powered to identify such differences (45). In addition, many studies excluded patients with mobile spondylolistheses or unstable segments. Limiting surgical burden by withholding fusion in these patients remains unsupported.
Surgery including fusion when indicated can provide improvement in pain and function, with high satisfaction rates regardless of age. There is evidence, though weak, to suggest that age should not be used as a criterion to avoid fusion with instrumentation in the elderly. Care should be taken to avoid a less invasive surgery if there is a high risk of early failure. Indeed, the most common indications for revision were recurrent or residual stenosis and instability. Other studies however provide evidence, though also weak, that increased surgical invasiveness can lead to higher rates of complication in elderly patients. Surgeons must remain circumspect about the risks and benefits of these procedures.
Improving the safety and efficacy of surgery in the elderly
Newer surgical techniques and changes in perioperative management have been proposed to limit the impact of surgery on elderly patients and reduce their risks for complication. One such option is less or minimally invasive spine surgery (MISS). The typical goal of MISS is to reduce physiologic and anatomic disruption from surgery while achieving the same goals of an open approach. MISS approaches for the lumbar spine seek to limit the surgical burden and allow for earlier recovery and improved function, with reduced blood loss, pain, length of stay, and complications. The value of MISS when applied judiciously might be amplified in an elderly population by reducing perioperative physiologic demand and injury while allowing earlier return to activity. These approaches with modifications in anesthetic techniques and perioperative care may directly address the concerns of surgery in the elderly.
Rosen et al. evaluated 50 patients aged ≥75 who underwent a minimally invasive spine decompression with endoscopy or a tubular retractor (52). No patients had a major complication, and there were no deaths. In this study, as in some prior studies (33), patient aged over 80 had the greatest improvement in symptoms versus younger patients. Son et al. found similar results between elderly patients age >65 and younger patients undergoing endoscopic transforaminal lumbar discectomies (53). Minimally invasive spine fusion techniques have shown similar benefits for elderly patients. Goh et al. evaluated the outcomes of 39 patients ≥70 versus 129 younger patients undergoing MISS-TLIF for lumbar degenerative spondylolisthesis (54). Outcomes were similar at 2 years, with equivalent rates of satisfaction and equivalent fusion rates. Complications were low and similar between groups. Avila et al. reviewed the results of 26 elderly patients over age 65 who underwent six different types of procedures considered MISS including lateral lumbar interbody fusion in addition to variations on other decompression and interbody fusion procedures (55,56). Complications were reported at 11.1% with improvement in function and pain.
Criticisms of some available approaches include high cost and complexity, challenging leaning curves, unique complication profiles, and potential limitations in surgical benefit. As techniques mature however, more rigorous study is required to identify the benefits and limitations of MISS in the elderly population.
Beyond surgical technique, anesthetic technique has been evaluated for the potential to reduce surgical morbidity and complications in the elderly. Modifications to anesthetic medication regimen, procedure length, use of regional blocks and avoidance of general anesthetics with “awake” surgery under local or spinal anesthetic have begun to show promise. Lessing et al. for example evaluated 56 patients aged over 70 who underwent decompression and fusion or decompression alone under a spinal anesthetic (57). There were no major complications and there was no need to convert to general anesthesia. The authors suggested a time limit of 3.5 hours. They completed a comparison study to general anesthesia that found decreased blood loss with decreased odds of blood transfusion, lower pain scores, and similar rates of complication (57). In a similar study, Wang et al. evaluated 424 cases performed under spinal anesthetic in patients aged ≥80 years without increased rates of complication (58).
Other efforts have been made in preoperative optimization. Optimizing chronic conditions and avoiding surgical episodes during acute exacerbations has been beneficial for young and elderly patients alike. Care for obesity, nutrition, glucose control, anemia, bone density, tobacco use, and opioid use or other psychosocial factors can improve outcomes, reduce variability, and decrease costs (59). Osteoporosis will increase in proportion with the shifting demographics, as approximately 26% of women older than 65 years of age and in 50% of those older than 85 have osteoporosis. Osteoporosis can affect fixation in instrumented cases, subsidence, and deformity progression. Close management of osteoporosis may limit these impacts on clinical outcomes. Preoperative optimization requires a multidisciplinary approach to address modifiable risk factors and monitor antiresorptive or anabolic medications. Most studies support use of antiresorptive agents through the course of fusion, including bisphosphonates and denosumab (60). The specific indications and contraindications for parathyroid hormone and sclerostin inhibitors vary; however, there is evidence for improved fusion rates and decreased mechanical complications with 3–6 months of preoperative therapy (20).
Enhanced recovery after surgery (ERAS) programs have been developed for improving perioperative care and efficiency for elderly patients following spine surgery. Such programs often include pre-, peri- and postoperative optimization and risk reduction, often with multidisciplinary teams including surgeons, anesthesiologists, as well as hospitalist or geriatric inpatient co-management (61). For example, the Perioperative Optimization of Senior Health (POSH) program was launched with the aim of improving outcomes in elderly patients undergoing complex lumbar spine surgery. This program includes preoperative evaluation, hospitalist and geriatric co-management, and coordinated multidisciplinary rehabilitation (61). One hundred patients undergoing lumbar decompression and fusion in the POSH program were compared to 25 matched patients before implementation of the program. Length of stay decreased by 30%, and patients were found to have increased ambulation rates with increased home discharge. In a similar ERAS program for elderly patients, Cui et al. evaluated the results of patients aged >75 before versus after implementation of their program undergoing multilevel lumbar fusion (62). They implemented pre-, intra- and postoperative modifications in care to optimize nutrition, prophylaxis, anesthesia and early recovery. Pain scores and length of stay were lower during admission without a change in complication rates. Wang et al. also evaluated an ERAS program for elderly patients undergoing 1- or 2-level lumbar fusions (63). Complications, mortality rates, and pain and functional outcomes did not differ; however, there was a decrease in length of stay. As length of stay and discharge disposition were prognostic of complications and outcome in prior studies (42), ERAS programs may be even more relevant in the elderly population.
Reducing surgical invasiveness and physiologic burden will be crucial in improving the safety and efficacy of lumbar spine surgery in elderly patients. Less invasive surgical and anesthetic techniques, perioperative optimization, and perioperative care are all important to achieve these goals for patients of all ages, but promise greater benefits to older patients with higher rates of comorbidity. Further study is needed to identify intraoperative factors that may have a greater impact on the elderly population. Until more data is available to identify more standard patters of care however, surgical decision-making on a case-by-case basis will hold an outsized role in outcomes.
Representative cases
Representative cases were chosen to illustrate the approaches to surgical management of lumbar pathology in elderly patients.
Case 1
An 82-year-old man with hypertension, atrial fibrillation, and prior deep vein thrombosis on apixaban and a 2-year history of increasing low back and left leg pain presented for surgical consultation. He had experienced radiating left leg pain at both the left buttock as well as the anterior thigh, and distal radiation to the dorsal and medial foot and ankle with running. Symptoms were claudicating. He had excellent rest relief with sitting and supine positioning. Due to his symptoms, he had stopped running completely 6 months ago. He had maintained a high functional capacity prior to symptoms worsening. He had no neurologic weakness on physical examination.
For the past 2 years, he had managed his symptoms with activity modification, physical therapy, and medications including diclofenac gel and gabapentin 300 mg three times daily. He had undergone left L3 and L4 transforaminal epidural steroid injections with initial relief and subsequent return of symptoms.
Radiographs demonstrated a 25-degree degenerative lumbar scoliosis with mild L4–5 spondylolisthesis (Figure 1A). A lumbar magnetic resonance imaging (MRI) confirmed stenosis greatest centrally from L2–5, with foraminal stenosis moderate at L2–3 and L3–4 on the left, correlating with his distributions of pain (Figure 1B).

Decompression alone versus decompression with instrumented fusion were discussed. The patient elected decompression alone. He was reevaluated by his primary care physician and cardiologist. With no other factors to optimize on this evaluation and his apixaban held perioperatively, he then underwent bilateral decompressions via a unilateral approach with foraminotomies of the left L2–4 roots. The midline structures were preserved. There were no perioperative complications. He was discharged home on the day of surgery.
The patient had early and durable improvement in leg pain for 1 year of follow-up. Subsequent radiographs found settling at the L3–4 disc (Figure 1C); however, radicular symptoms did not recur. He was satisfied with his outcome.
Case 2
An 85-year-old woman with diabetes mellitus, hypertension and stage 2 chronic kidney disease presented for evaluation of worsening back and bilateral leg pain worsening in the past 2–3 years, but ongoing for at least two decades. Pain was severely claudicating, with more tolerable symptoms on sitting. She had begun to feel progression of weakness in the legs as well. She had ankle dorsiflexion and great tow weakness bilaterally graded 4/5. She had difficulty standing fully upright due to the severity of her leg pain.
Prior conservative treatment had been extensive over years, with activity modification, physical therapy, medications, injections, and alternatives including chiropractic trialed over the years without persistent improvement.
Radiographs demonstrated anterolistheses of L3–4 and L4–5 with difficultly with lumbar extension (Figure 2A). A lumbar MRI confirmed stenosis at both L3–4 and L4–5 with mild foraminal stenosis (Figure 2B). The spondylolistheses were stable from supine to standing imaging and the facets were partially locked.
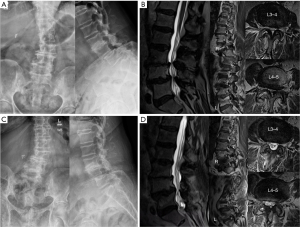
Decompression alone versus decompression with instrumented fusion were discussed. The patient elected decompression alone. She was evaluated by her primary care physician. Her glucose control was optimized, and her other comorbidities were well controlled. She then underwent partial laminectomies from L3–5 preserving the midline structures at L4–5. The patient was admitted following surgery with hospitalist co-management. She ambulated postoperative day 0, and glucose control was maintained. There were no perioperative complications. She discharged home 3 days after surgery
The patient had early improvement with near resolution of leg pain postoperatively and at a 2-week wound check. However, leg pain then returned over the following 2 months, and become severe again by 3 months postoperatively. Physical therapy, medications, and repeat L4 and L5 transforaminal epidural steroid injections were attempted, however pain persisted. Repeat radiographs found further with settling and anterolisthesis particularly at L4–5 (Figure 2C). A subsequent MRI at 6 months found worsening foraminal stenosis (Figure 2D). The patient was offered revision to an interbody fusion; however, she deferred this and had maintained nonsurgical management at 2 years after decompression.
Case 3
An 87-year-old woman with hypertension, hyperlipidemia, and osteoporosis and a decades-long history of low back and now more predominant and worsening radiating left lateral leg pain presented for surgical consultation. Pain was claudicating, improving with sitting. She was not concerned about her coronal or sagittal imbalance. Prior conservative treatment had included activity modification, physical therapy, medications, and epidural injections.
Radiographs demonstrated a degenerative scoliosis with a prominent fractional curve and degeneration of the left facet at L5–S1 (Figure 3A). A lumbar MRI confirmed foraminal stenosis on the left at L5–S1 (Figure 3B).
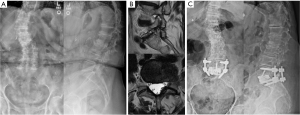
Decompression alone versus decompression with instrumented fusion were discussed. The patient was recommended to undergo an interbody fusion to reestablish foraminal height at the foramen. She was evaluated by her primary care physician. She had a left hip T-score of −2.8 and was started on calcium, vitamin D and teriparatide for 6 months. She then underwent an L5–S1 ALIF with posterior spinal fusion in a single lateral decubitus position. The patient was admitted following surgery with hospitalist co-management. She ambulated postoperative day 0. Postoperative radiographs found improved alignment of L5–S1 (Figure 3C). There were no perioperative complications. She discharged home 2 days after surgery.
The patient had immediate and significant improvement in her radiating leg pain. Her presenting symptoms had resolved by 6-week follow-up, and remained durable for 2 years of follow-up. She was satisfied with her outcome.
Discussion
Elderly patients present a challenge to the healthcare system as their proportion of the population increases. This demographic shift is expected to increase the prevalence of symptomatic degenerative lumbar pathology in a population with higher perioperative risk (2,14). The demand for lumbar spine surgery for elderly patients is expected to rise further as functional capacity and expectations are maintained later into life. Concerns persist regarding perioperative efficacy and safety for such patients (5-7). Current evidence is variable yet more positive than these concerns suggest, although limitations and deficiencies in the data remain. Most studies suggest that lumbar spine surgery remains safe and effective for select and well optimized patients with degenerative pathology in comparison to younger patients (25-27). Even studies that report higher complication rates typically argue for continued accessibility of surgery even for super-elderly patients over age 80 when appropriate nonsurgical management has failed given the benefits of surgery (29-39). Some studies even suggest greater clinical benefit in more elderly patients (37,52). These results provide elderly patients with options for their care when nonsurgical management fails (21). However, with weaker quality of evidence and the potential for complication and harm, elderly patients must be evaluated individually. Appropriate care requires informed patients engaged in shared decision-making.
Use of fusion techniques and instrumentation, when appropriately indicated, has also had variable association with complications in elderly patients (43,44). Clearly, increased invasiveness, levels included, surgical duration, and blood loss are associated with complications in this population (23,24,28,33). Careful decision-making is therefore required to limit surgical burden while also limiting failure. Reducing the surgical burden with less invasive surgical and anesthetic techniques as well as perioperative optimization and management will help to further mitigate potential harms of surgery and may be particularly advantageous for elderly patients. These interventions are pivotal in directly addressing surgical risk in the elderly.
Studies of lumbar spine surgery in elderly populations remain limited by small sample sizes, heterogeneous populations and interventions, and selection biases. This narrative review consequently has limitations as well due to the heterogeneity of the literature. This was a limited review without new statistical analysis of the topic including largely retrospective clinical studies in which patient selection was nonrandomized and therefore subject to surgeon assessment of patient candidacy for surgical intervention. Most studies include, for example, elderly patients undergoing surgery who have been assessed preoperatively and found to be medically stable to proceed or were optimized prior to the intervention. The methodology of complication data collection was also variable between studies. Furthermore, there is a paucity of high-quality studies evaluating the utility of MISS approaches specifically among the elderly.
Due to the limitations in the literature, representative cases were chosen to illustrate the approaches to surgical management of lumbar degenerative pathology in elderly patients. Each patient had failed extensive nonsurgical management and had completed preoperative assessment and optimization with perioperative programs coordinated to reduce risk and complications. The patients in cases 1 and 3 included stable deformities, however had success with both decompression versus decompression and fusion. The patient in case 2 had an early failure associated with progression of instability and recurrent stenosis. Given the broad variability of symptoms, anatomy, and expectations in the elderly, surgical interventions are likely best considered on a case-by-case basis. Cautious and observant workup, planning and shared decision-making are required to improve clinical outcomes and avoid harm in these elderly patients.
Conclusions
The growing elderly population presages an increase in degenerative spinal pathology and consequently demand for lumbar spine surgery. This review found that lumbar surgery can provide safe and durable improvements in pain, function, and quality of life for well optimized elderly patients. Weak evidence supports surgery also in the super-elderly, although older age and the comorbidities associated with it increase surgical risk in this population. Increased risk was found for surgery for some super-elderly patients, and surgery should be indicated with caution in increasingly older patients. Surgical invasiveness is associated with higher rates of surgical complications, however elderly patients still benefit from fusion and instrumentation when properly indicated. Spine surgeons must be prepared to manage an increasingly challenging and medically complex elderly population with higher expectations for outcomes and quality of life. Implementing programs for perioperative optimization reduces outcome variability and supports these goals. Given the weaknesses of the retrospective studies making up the bulk of the spine literature including elderly patients, further prospective studies are needed to better address the risks and benefits of surgery for this vulnerable population.
Age alone is not a contraindication for lumbar spine surgery. Elderly patient must be informed of risks associated with age, but should also be aware that surgery remains an option with studies reporting safety and efficacy similar to younger patients. Until the quality of evidence improves, surgical decision-making should remain case-by-case to safely achieve patients’ goals.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Mark Lambrechts and Brian Karamian) for the series “Degenerative Spine Disease” published in AME Medical Journal. The article has undergone external peer review.
Reporting Checklist: The author has completed the Narrative Review reporting checklist. Available at https://amj.amegroups.com/article/view/10.21037/amj-23-150/rc
Peer Review File: Available at https://amj.amegroups.com/article/view/10.21037/amj-23-150/prf
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj-23-150/coif). The series “Degenerative Spine Disease” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- He W, Goodkind D, Kowal P. An aging world: 2015. United States Census Bureau; 2016:1-175.
- Deyo RA, Gray DT, Kreuter W, et al. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005;30:1441-5; discussion 1446-7. [Crossref] [PubMed]
- Bae HW, Rajaee SS, Kanim LE. Nationwide trends in the surgical management of lumbar spinal stenosis. Spine (Phila Pa 1976) 2013;38:916-26. [Crossref] [PubMed]
- Zhu K, Devine A, Dick IM, et al. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine (Phila Pa 1976) 2007;32:2012-8. [Crossref] [PubMed]
- Graham J. Research helps seniors make informed decisions about risks, benefits of major surgery. Kaiser Health News. 2022 Nov 25. Available online: https://www.cnn.com/2022/11/25/health/seniors-major-surgery-khn-partner/index.html
- Span P. The Elderly Are Getting Complex Surgeries. Often It Doesn’t End Well. The New York Times. 2019 Jun 7. Available online: https://www.nytimes.com/2019/06/07/health/elderly-surgery-complications.html
- Span P. Frail Older Patients Struggle After Even Minor Operations. The New York Times. 2019 Dec 13. Available online: https://www.nytimes.com/2019/12/13/health/frail-elderly-surgery.html
- Zimmer Z, Rubin S. Life Expectancy With and Without Pain in the U.S. Elderly Population. J Gerontol A Biol Sci Med Sci 2016;71:1171-6. [Crossref] [PubMed]
- Försth P, Ólafsson G, Carlsson T, et al. A Randomized, Controlled Trial of Fusion Surgery for Lumbar Spinal Stenosis. N Engl J Med 2016;374:1413-23. [Crossref] [PubMed]
- France JC, Yaszemski MJ, Lauerman WC, et al. A randomized prospective study of posterolateral lumbar fusion. Outcomes with and without pedicle screw instrumentation. Spine (Phila Pa 1976) 1999;24:553-60. [Crossref] [PubMed]
- Harris RE. Epidemiology of Chronic Disease: Global Perspectives. Sudbury, ON: Jones & Bartlett Learning; 2013.
- Mullahy J. Live long, live well: quantifying the health of heterogeneous populations. Health Econ 2001;10:429-40. [Crossref] [PubMed]
- Boos N, Weissbach S, Rohrbach H, et al. Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo Award in basic science. Spine (Phila Pa 1976) 2002;27:2631-44. [Crossref] [PubMed]
- Whitmore RG, Stephen JH, Vernick C, et al. ASA grade and Charlson Comorbidity Index of spinal surgery patients: correlation with complications and societal costs. Spine J 2014;14:31-8. [Crossref] [PubMed]
- Wang SK, Mu H, Wang P, et al. The Charlson Comorbidity Index and depression are associated with satisfaction after short-segment lumbar fusion in patients 75 years and older. Front Surg 2022;9:991271. [Crossref] [PubMed]
- Veronesi F, Borsari V, Martini L, et al. The Impact of Frailty on Spine Surgery: Systematic Review on 10 years Clinical Studies. Aging Dis 2021;12:625-45. [Crossref] [PubMed]
- Kweh BTS, Lee HQ, Tan T, et al. Risk Stratification of Elderly Patients Undergoing Spinal Surgery Using the Modified Frailty Index. Global Spine J 2023;13:457-65. [Crossref] [PubMed]
- Kim JY, Park IS, Kang DH, et al. Prediction of Risk Factors after Spine Surgery in Patients Aged >75 Years Using the Modified Frailty Index. J Korean Neurosurg Soc 2020;63:827-33. [Crossref] [PubMed]
- Chotai S, Gupta R, Pennings JS, et al. Frailty and Sarcopenia: Impact on Outcomes Following Elective Degenerative Lumbar Spine Surgery. Spine (Phila Pa 1976) 2022;47:1410-7. [Crossref] [PubMed]
- Dodwad SM, Khan SN. Surgical stabilization of the spine in the osteoporotic patient. Orthop Clin North Am 2013;44:243-9. [Crossref] [PubMed]
- Tadokoro K, Miyamoto H, Sumi M, et al. The prognosis of conservative treatments for lumbar spinal stenosis: analysis of patients over 70 years of age. Spine (Phila Pa 1976) 2005;30:2458-63. [Crossref] [PubMed]
- Simotas AC, Dorey FJ, Hansraj KK, et al. Nonoperative treatment for lumbar spinal stenosis. Clinical and outcome results and a 3-year survivorship analysis. Spine (Phila Pa 1976) 2000;25:197-203; discussions 203-4.
- Deyo RA, Cherkin DC, Loeser JD, et al. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am 1992;74:536-43. [Crossref] [PubMed]
- Carreon LY, Puno RM, Dimar JR 2nd, et al. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am 2003;85:2089-92. [Crossref] [PubMed]
- Glassman SD, Carreon LY, Dimar JR, et al. Clinical outcomes in older patients after posterolateral lumbar fusion. Spine J 2007;7:547-51. [Crossref] [PubMed]
- Acosta FL, Cloyd JM, Aryan HE, et al. Perioperative complications and clinical outcomes of multilevel circumferential lumbar spinal fusion in the elderly. J Clin Neurosci 2009;16:69-73. [Crossref] [PubMed]
- Okuda S, Oda T, Miyauchi A, et al. Surgical outcomes of posterior lumbar interbody fusion in elderly patients. J Bone Joint Surg Am 2006;88:2714-20. [Crossref] [PubMed]
- Cloyd JM, Acosta FL Jr, Ames CP. Complications and outcomes of lumbar spine surgery in elderly people: a review of the literature. J Am Geriatr Soc 2008;56:1318-27. [Crossref] [PubMed]
- Raffo CS, Lauerman WC. Predicting morbidity and mortality of lumbar spine arthrodesis in patients in their ninth decade. Spine (Phila Pa 1976) 2006;31:99-103. [Crossref] [PubMed]
- Wang MY, Widi G, Levi AD. The safety profile of lumbar spinal surgery in elderly patients 85 years and older. Neurosurg Focus 2015;39:E3. [Crossref] [PubMed]
- Son HJ, Jo YH, Ahn HS, et al. Outcomes of lumbar spinal fusion in super-elderly patients aged 80 years and over: Comparison with patients aged 65 years and over, and under 80 years. Medicine (Baltimore) 2021;100:e26812. [Crossref] [PubMed]
- Gerhardt J, Bette S, Janssen I, et al. Is Eighty the New Sixty? Outcomes and Complications after Lumbar Decompression Surgery in Elderly Patients over 80 Years of Age. World Neurosurg 2018;112:e555-60. [Crossref] [PubMed]
- Balabaud L, Pitel S, Caux I, et al. Lumbar spine surgery in patients 80 years of age or older: morbidity and mortality. Eur J Orthop Surg Traumatol 2015;25:S205-12. [Crossref] [PubMed]
- Bouloussa H, Alzakri A, Ghailane S, et al. Is it safe to perform lumbar spine surgery on patients over eighty five? Int Orthop 2017;41:2091-6. [Crossref] [PubMed]
- Liu C, Guo C, Meng F, et al. Perioperative risk factors related to complications of lumbar spine fusion surgery in elderly patients. BMC Musculoskelet Disord 2023;24:573. [Crossref] [PubMed]
- Saleh A, Thirukumaran C, Mesfin A, et al. Complications and readmission after lumbar spine surgery in elderly patients: an analysis of 2,320 patients. Spine J 2017;17:1106-12. [Crossref] [PubMed]
- Arinzon ZH, Fredman B, Zohar E, et al. Surgical management of spinal stenosis: a comparison of immediate and long term outcome in two geriatric patient populations. Arch Gerontol Geriatr 2003;36:273-9. [Crossref] [PubMed]
- Rault F, Briant AR, Kamga H, et al. Surgical management of lumbar spinal stenosis in patients over 80: is there an increased risk? Neurosurg Rev 2022;45:2385-99. [Crossref] [PubMed]
- Rihn JA, Hilibrand AS, Zhao W, et al. Effectiveness of surgery for lumbar stenosis and degenerative spondylolisthesis in the octogenarian population: analysis of the Spine Patient Outcomes Research Trial (SPORT) data. J Bone Joint Surg Am 2015;97:177-85. [Crossref] [PubMed]
- Tan JY, Kaliya-Perumal AK, Oh JY. Is Spinal Surgery Safe for Elderly Patients Aged 80 and Above? Predictors of Mortality and Morbidity in an Asian Population. Neurospine 2019;16:764-9. [Crossref] [PubMed]
- Lagman C, Ugiliweneza B, Boakye M, et al. Spine Surgery Outcomes in Elderly Patients Versus General Adult Patients in the United States: A MarketScan Analysis. World Neurosurg 2017;103:780-8. [Crossref] [PubMed]
- McGirt MJ, Parker SL, Hilibrand A, et al. Lumbar Surgery in the Elderly Provides Significant Health Benefit in the US Health Care System: Patient-Reported Outcomes in 4370 Patients From the N2QOD Registry. Neurosurgery 2015;77:S125-35. [Crossref] [PubMed]
- Lee CH, Hyun SJ, Kim KJ, et al. Decompression only versus fusion surgery for lumbar stenosis in elderly patients over 75 years old: which is reasonable? Neurol Med Chir (Tokyo) 2013;53:870-4. [Crossref] [PubMed]
- Ragab AA, Fye MA, Bohlman HH. Surgery of the lumbar spine for spinal stenosis in 118 patients 70 years of age or older. Spine (Phila Pa 1976) 2003;28:348-53. [Crossref] [PubMed]
- Kilinçer C, Steinmetz MP, Sohn MJ, et al. Effects of age on the perioperative characteristics and short-term outcome of posterior lumbar fusion surgery. J Neurosurg Spine 2005;3:34-9. [Crossref] [PubMed]
- Endres S, Aigner R, Wilke A. Instrumented intervertebral or posterolateral fusion in elderly patients: clinical results of a single center. BMC Musculoskelet Disord 2011;12:189. [Crossref] [PubMed]
- Patel JY, Kundnani VG, Chawada B. Is Older Age a Contraindication for Single-Level Transforaminal Lumbar Interbody Fusion?. Asian Spine J 2021;15:447-54. [Crossref] [PubMed]
- Tsujimoto T, Itoga R, Kanayama M, et al. Clinical outcomes of short-segment lumbar fusion in patients older than 85 years with a minimum 2-year follow-up. J Neurosurg Spine 2023;39:40-6. [Crossref] [PubMed]
- Cassinelli EH, Eubanks J, Vogt M, et al. Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine (Phila Pa 1976) 2007;32:230-5. [Crossref] [PubMed]
- Becker P, Bretschneider W, Tuschel A, et al. Life quality after instrumented lumbar fusion in the elderly. Spine (Phila Pa 1976) 2010;35:1478-81. [Crossref] [PubMed]
- Tu P, Cao S, Jiang C, et al. A comparative study of Lumbar Decompression and Fusion with Internal Fixation versus Simple Decompression in elderly patients with two-segment Lumbar Spinal Stenosis. Pak J Med Sci 2021;37:256-60. [PubMed]
- Rosen DS, O'Toole JE, Eichholz KM, et al. Minimally invasive lumbar spinal decompression in the elderly: outcomes of 50 patients aged 75 years and older. Neurosurgery 2007;60:503-9; discussion 509-10. [Crossref] [PubMed]
- Son S, Yoo BR, Kim HJ, et al. Efficacy of Transforaminal Endoscopic Lumbar Discectomy in Elderly Patients Over 65 Years of Age Compared to Young Adults. Neurospine 2023;20:597-607. [Crossref] [PubMed]
- Goh GS, Tay YWA, Liow MHL, et al. Elderly Patients Undergoing Minimally Invasive Transforaminal Lumbar Interbody Fusion May Have Similar Clinical Outcomes, Perioperative Complications, and Fusion Rates As Their Younger Counterparts. Clin Orthop Relat Res 2020;478:822-32. [Crossref] [PubMed]
- Avila MJ, Walter CM, Baaj AA. Outcomes and Complications of Minimally Invasive Surgery of the Lumbar Spine in the Elderly. Cureus 2016;8:e519. [Crossref] [PubMed]
- Daubs MD, Lenke LG, Bridwell KH, et al. Decompression alone versus decompression with limited fusion for treatment of degenerative lumbar scoliosis in the elderly patient. Evid Based Spine Care J 2012;3:27-32. [PubMed]
- Lessing NL, Edwards CC 2nd, Dean CL, et al. Spinal Anesthesia for Geriatric Lumbar Spine Surgery: A Comparative Case Series. Int J Spine Surg 2020;14:713-21. [Crossref] [PubMed]
- Wang AY, Olmos M, Ahsan T, et al. Safety and feasibility of spinal anesthesia during simple and complex lumbar spine surgery in the extreme elderly (≥80 years of age). Clin Neurol Neurosurg 2022;219:107316. [Crossref] [PubMed]
- Maitra S, Mikhail C, Cho SK, et al. Preoperative Maximization to Reduce Complications in Spinal Surgery. Global Spine J 2020;10:45S-52S. [Crossref] [PubMed]
- Zhang AS, Khatri S, Balmaceno-Criss M, et al. Medical optimization of osteoporosis for adult spinal deformity surgery: a state-of-the-art evidence-based review of current pharmacotherapy. Spine Deform 2023;11:579-96. Erratum in: Spine Deform 2023;11:523. [Crossref] [PubMed]
- Adogwa O, Elsamadicy AA, Vuong VD, et al. Geriatric comanagement reduces perioperative complications and shortens duration of hospital stay after lumbar spine surgery: a prospective single-institution experience. J Neurosurg Spine 2017;27:670-5. [Crossref] [PubMed]
- Cui P, Wang P, Kong C, et al. Patients Older Than 75 Years Undergoing Polysegmental Lumbar Fusion Surgery Can also Benefit from Enhanced Recovery After Surgery Program. Clin Interv Aging 2022;17:245-52. [Crossref] [PubMed]
- Wang P, Wang Q, Kong C, et al. Enhanced recovery after surgery (ERAS) program for elderly patients with short-level lumbar fusion. J Orthop Surg Res 2020;15:299. [Crossref] [PubMed]
Cite this article as: Kleimeyer JP. A narrative review of treatment of the elderly patient: do we need to alter surgical management of lumbar spine disease? AME Med J 2024;9:7.

