Primary mucosa associated lymphoid tissue (MALT) B-cell lymphoma—a rare breast malignancy
Case
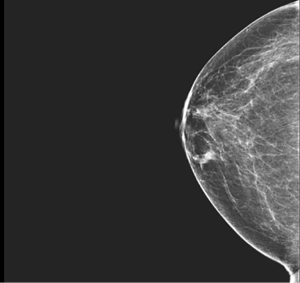
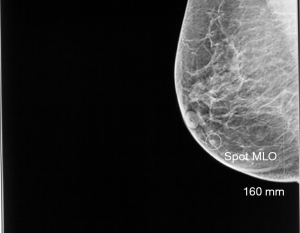
An 82-year-old African American female underwent a screening mammogram which demonstrated a subcentimeter right lower inner quadrant mass (Figures 1 and 2). Physical exam did not demonstrate any palpable masses or adenopathy. Additional imaging with a targeted ultrasound demonstrated a 0.3 cm hypoechoic abnormality at 3 o’clock in the right breast, for which she subsequently underwent an ultrasound guided core needle biopsy. Pathology showed lymphoid aggregates, mild fibrocystic changes including fibrosis, dilated ducts and periductal chronic inflammation, but no evidence of malignancy or atypia. The results were suspicious, however, for a reactive lymphoid infiltrate and the patient was referred for surgical consultation. She had an excisional biopsy of her right breast lesion with needle localization with pathology demonstrating atypical lymphoid infiltrate consistent with low grade B-cell MALT lymphoma, with no evidence of primary breast malignancy. Further confirmatory testing with immunohistochemistry was performed that demonstrated lymphocytes that were dominantly B cells admixed with some T cells. The B-cells were positive for BCL2, but negative for CD5, CD10, CD23 and CD43. Immunoglobulin heavy chain gene rearrangement assay by PCR and electrophoresis revealed positive B-cell monoclonality.
After the initial diagnosis, the patient underwent staging with CT scan of the chest, abdomen and pelvis that not demonstrate any additional lymphadenopathy. An esophagoduodenoscopy (EGD) was also performed which showed mild chronic gastritis. Random gastric biopsies were negative for H. Pylori, and immunostains show some mixed T-cells and B-cells of small lymphoid aggregates. Colonoscopy also did not reveal any masses or evidence of MALT lymphoma. A bone marrow biopsy was deferred as the patient declined.
Post-operatively, she underwent adjuvant radiation therapy with a total dose of 6,040 cGy over four weeks. She also received four doses of Rituximab over four weeks, which she tolerated well. On routine follow up, she is doing well, asymptomatic, and denies pain, discharge or masses in her right breast. On exam, she has a well healed incision, and has no palpable masses in her right breast. She does, however complain of fatigue and myalgia, with elevated ESR of 120, suspicious for polymyalgia rheumatica.
Discussion
Primary breast lymphomas (PBLs) are uncommon manifestations of breast cancer and account for 0.4% to 0.5% of all breast malignancies (1). When in the breast, PBLs commonly presents as painless masses in the breast, but they can also present with local pain or inflammation, palpable lymph nodes, and incidental findings on screening mammography (1-4).
There are two broader categories, one of which is unilateral, more commonly seen in the right breast with an indolent course, in an age group consistent with breast cancer, and the second in lactating younger women with bilateral predominance, and aggressive disseminating course (5). The former type presents typically in the fifth to sixth decade of life, and accounts for about 84% of the cases described in the literature (1,5). Within the broad group of PBL, there are several different types including diffuse B-cell lymphoma, anaplastic large cell lymphoma, Burkett’s lymphoma, mantle cell, follicular, and marginal zone lymphoma (6). Following diagnosis, prognosis mostly depends on the lymphoma subtype—indolent vs. aggressive. More favorable outcomes have been seen in primary MALT B-cell lymphoma (PM-BCL), with five-year survival can be as high as 91% (7).
Specifically, mucosa associated lymphoid tissue (MALT) lymphomas account for 12% of all PBLs, and shares histopathologic characteristics with marginal zone B cell lymphomas (2,8). MALT lymphomas are extranodal indolent lymphomas that can present in a variety of organs including stomach, small or large bowels, lungs, salivary glands, thyroid, skin, thymus, tonsils, liver, kidney, bladder, and the breast (1). On histology, MALT lymphomas demonstrated oval or indented nuclei with varying degrees of cytoplasmic clearing, with immuno-histochemistry staining positive for CD 20 & BCL-2, as well as CD43, CD10, and CD5 (5,9). It has been suggested that the lymphocytic infiltrates found in MALT B-cell lymphoma is similar in pathophysiology as other autoimmune disease with lymphocytic predominance, such as Hashimoto’s thyroiditis, Sjogren’s, or diabetes (9,10). Interestingly, our patient has symptoms of fatigue and myalgia with elevated ESR, possibly due to polymyalgia rheumatica, from an elevated inflammatory response for which she is currently being worked up.
Patients with primary MBCL, should also undergo testing to rule out other primary sources of cancer, as the breast could be a site of metastasis for primary MALT of the gastrointestinal tract, or other primary site. Imaging should be obtained, and EGD & colonoscopy performed—in this particular case, her GI workup was negative for malignancy. Staging should include whole body positron emission tomography with computed tomography (PET-CT) and bone marrow biopsy. In select patients with diffuse type B-cell lymphoma, CSF fluid should also be tested for possible central nervous system involvement (6).
Treatment strategies involve local excision along with chemoradiation therapy targeted towards specific clonal antibodies. Multiple series have shown that surgery alone confers inferior survival compared to immunotherapy and radiotherapy, and that surgery should be limited to excisional biopsy (6). Most retrospective studies focus on outcomes in primarily diffuse large B-cell lymphoma of the breast, and the treatment regimens are focused on CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) therapy +/− radiotherapy or +/− Rituximab (R-CHOP) with 5-year survival rates ranging between 50–70%, demonstrating improved outcomes with combined R-CHOP and radiotherapy (6,7). High risk patients, with aggressive type lymphoma, 5-year survival was improved with 4–6 cycles of chemotherapy, suggesting a dose-relationship benefit (6). Another study looking at indolent type PBCL demonstrated that 88% of patients responded to initial radiotherapy +/− surgery alone, without initiation of chemotherapy, and 5-year local regional control of 92%. Overall survival in these patients over 5 years was 75% (7). In patients with more aggressive disease, treated with R-CHOP + radiotherapy demonstrated a non-significant survival benefit to just CHOP + radiotherapy alone (78% vs. 49%, P=0.14).
Current treatment strategies advocate for dividing patients into either an indolent vs. aggressive lymphoma category. For both patients, surgery seems to play a limited role in treatment. Those that have indolent disease are primary treated with radiotherapy first with good locoregional control and 5-year survival. Patients with higher risk lymphomas were benefited from more aggressive chemoradiotherapy, which increased survival rates compared to radiotherapy alone. PM-BCL seems to fall into the category of indolent lymphomas, and should be treated initially with radiotherapy alone (7). Close follow up and increased patient series looking specifically at treatment regimens targeted at PM-CBL patients will need to be conducted to ascertain best treatment outcomes and practices.
Conclusions
Despite the increasing number of reported cases, experience with PBL remains limited within institutions, and there is no consensus on best treatment practices. It is important to keep PBL in the differential for breast lesions showing lymphocytic infiltrates on core needle biopsy with no evidence of carcinoma, and obtain appropriate immunohistochemical staining for B & T cells, in addition to PCR analysis for monoclonality (5,9). Treatment strategies involve local excision along with chemoradiation therapy targeted towards specific clonal antibodies.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/amj.2016.12.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gopal S, Awasthi S, Elghetany MT. Bilateral breast MALT lymphoma: a case report and review of the literature. Ann Hematol 2000;79:86-9. [Crossref] [PubMed]
- Rajendran RR, Palazzo JP, Schwartz GF, et al. Primary mucosa-associated lymphoid tissue lymphoma of the breast. Clin Breast Cancer 2008;8:187-8. [Crossref] [PubMed]
- Kim DH, Jeong JY, Lee SW, et al. 18F-FDG PET/CT finding of bilateral primary breast mucosa-associated lymphoid tissue lymphoma. Clin Nucl Med 2015;40:e148-9. [Crossref] [PubMed]
- Jeanneret-Sozzi W, Taghian A, Epelbaum R, et al. Primary breast lymphoma: patient profile, outcome and prognostic factors. A multicentre Rare Cancer Network study. BMC Cancer 2008;8:86. [Crossref] [PubMed]
- Hugh JC, Jackson FI, Hanson J, et al. Primary breast lymphoma. An immunohistologic study of 20 new cases. Cancer 1990;66:2602-11. [Crossref] [PubMed]
- Cheah CY, Campbell BA, Seymour JF. Primary breast lymphoma. Cancer Treat Rev 2014;40:900-8. [Crossref] [PubMed]
- Caon J, Wai ES, Hart J, et al. Treatment and outcomes of primary breast lymphoma. Clin Breast Cancer 2012;12:412-9. [Crossref] [PubMed]
- Joks M, Myśliwiec K, Lewandowski K. Primary breast lymphoma - a review of the literature and report of three cases. Arch Med Sci 2011;7:27-33. [Crossref] [PubMed]
- Farinha P, André S, Cabeçadas J, et al. High frequency of MALT lymphoma in a series of 14 cases of primary breast lymphoma. Appl Immunohistochem Mol Morphol 2002;10:115-20. [Crossref] [PubMed]
- Gupta D, Shidham V, Zemba-Palko V, et al. Primary bilateral mucosa-associated lymphoid tissue lymphoma of the breast with atypical ductal hyperplasia and localized amyloidosis. A case report and review of the literature. Arch Pathol Lab Med 2000;124:1233-6. [PubMed]
Cite this article as: Shao JM, Cheney M, Oppong BA. Primary mucosa associated lymphoid tissue (MALT) B-cell lymphoma—a rare breast malignancy. AME Med J 2016;1:5.